Some nursing mothers, according to indications, are forced to take medications, including antibacterial drugs. Almost all substances pass through the blood into breast milk and affect the baby. In case of serious pathologies, it is important to choose the appropriate drug, but some doctors prefer to treat patients with a decoction of herbs instead of proper therapy, for fear of harming the baby. Find out which antibiotics are not harmful when breastfeeding and what rules should be followed so as not to harm the baby.
antibiotics during breastfeeding
When are antibiotics needed?
The action of antibacterial drugs is aimed at inhibiting bacteria.
I saw doctors who, when they said “I’m breastfeeding,” nervously crossed out prescriptions and insisted that medications were prohibited during this period. The poor mother was advised to drink tea with honey, soar her feet, put on cupping - anything, just not to take responsibility for the treatment, sending her to coordinate this with the pediatrician.
A nursing mother is an ordinary patient, more susceptible to infections: she gives all the beneficial substances to the baby with milk, leaving her body without protection.
Sore throat during breastfeeding, bronchitis, cystitis and other inflammatory processes are common during this period of life.
When should you take antibacterial drugs?
- acute intestinal infection;
- diseases of the urinary system;
- postoperative complications;
- respiratory diseases, sinusitis, otitis, laryngitis, pharyngitis of bacterial etiology;
- purulent mastitis.
Never go against the doctor's recommendations - these are conditions that can be life-threatening for the mother.
Folk remedies for worms during breastfeeding

Folk remedies for worms during breastfeeding
Treatment of worms in hepatitis B can be carried out using products prepared according to traditional medicine recipes. Compositions based on medicinal herbs are gentle and practically do not cause side effects. However, even they are not always safe for the body of a nursing mother, so it is recommended to consult a doctor before using them.
We invite you to familiarize yourself with a selection of recipes that have been tested by more than one generation:
- Carrot juice. Peel the carrots, cut into small pieces and grind in a blender or juicer. Drink a glass of the resulting mixture daily before meals.
- Garlic. Eat a clove of garlic before and after meals. Be careful - if you eat too much garlic, you can cause a stomach burn.
- Enemas based on garlic and wormwood. Take wormwood and garlic in equal proportions, chop and pour boiling water. Leave for half an hour, then strain and use as an enema. Repeat the procedure once a day for 3-5 days.
- Pumpkin seeds. Grind 3 tablespoons of pumpkin seeds and eat on an empty stomach. 2 hours after this, drink 2 tablespoons of olive oil. The latter will act as a mild and safe laxative and the parasites will leave the body themselves along with the feces.

carrot juice
Garlic
Wormwood
Pumpkin seeds - Papaya (juice) and apple cider vinegar. Mix the ingredients in a 3:1 ratio and drink half a glass for a week. To cleanse the body faster, it is recommended to increase your water intake.
- Onion. Take a large onion and cut into small pieces. Place in a deep container and leave for 12 hours. Drink the resulting infusion on an empty stomach for 3-4 days.
- Walnuts (green). Peel the fruits and chop. Scoop 4 tablespoons of chopped nuts and pour boiling water over it. Add a pinch of salt and stir. Leave for an hour, strain. Drink 250 ml. composition, and after 2 hours - 2 tbsp. spoons of olive oil.

Papaya juice
Apple vinegar
Onion
Green walnuts
Before using folk remedies, it is recommended to visit an allergist and undergo an allergic reaction test.
Harm of antibiotics during breastfeeding
Medicines taken during breastfeeding are dangerous for the baby. What exactly is their harm?
- Allergic reactions of delayed and immediate type. This is important to consider, especially if the baby is less than a year old (after all, during this period the intestines, through which all substances are absorbed, are not fully developed and allow most of the allergens into the child’s blood).
- Accumulation in the body and exerting a toxic effect on the organs of the urinary system.
- Harmful effects on bone tissue and formation of dental stains.
- Changes in intestinal flora (the most likely effect of antibiotics during breastfeeding).
- Impact on systems and organs, changes in blood formula.
The medications that a nursing mother takes have an effect on the baby, but these are rare exceptions and not the rule.
If a nursing mother has been prescribed medications that are incompatible with breastfeeding
If the mother wants to continue breastfeeding, then the main thing that needs to be done is to try to find out for sure whether this medicine has analogues that are compatible with breastfeeding. Such analogues often exist, but many doctors simply do not take this into account when prescribing treatment.
For example, many doctors recommend temporary weaning when prescribing antibiotics, because this may harm the baby's intestinal flora. However, switching to formula alone will not have the best effect on the baby’s flora, and add to this the risk of further breast abandonment... At the same time, quite a few antibiotics are compatible with breastfeeding - for example, penicillins, cephalosporins, macrolides.
In addition, in some cases, the medicine is contraindicated during breastfeeding, not because it has a bad effect on the child, but because it reduces lactation as such - but few people delve into these subtleties, as well as the fact that for the mother the very continuation is often essential feeding, rather than a slightly reduced milk volume. If the doctor insists on one single drug, and suggests stopping feeding while taking it, it is best to find an opportunity to consult with another doctor, not to mention prescribing the first one.
If you have been prescribed a drug whose effect on breastfeeding you are not sure of, even if the annotation lists lactation as a contraindication, if possible, it is better to try to clarify the information from independent sources. The fact is that in the annotations for medicines in Russia they often write about the need to stop breastfeeding only because expensive tests are necessarily carried out to allow the use of a medicine while breastfeeding. Many manufacturers prefer to save on these tests by simply writing about the need to stop breastfeeding.
What medications should you not take while breastfeeding?
There is a list of antibacterial drugs that are strictly prohibited for lactating women, and if prescribed by a doctor, it is better to interrupt breastfeeding.
Don’t think that a mother’s illness is a reason to deny her child healthy nutrition.
If treatment is required, you can temporarily transfer the baby to artificial nutrition: pump so that the milk does not disappear. After the time has passed, when the drug is completely eliminated from the blood, continue breastfeeding again.
To prevent your baby from refusing to breastfeed:
- you need to choose a bottle with a nipple that resembles the natural shape of a nipple;
- feed on demand;
- if the heir does not take the breast, feed expressed milk through a bottle.

antibiotics during breastfeeding
Prohibited antibiotics during breastfeeding:
Drugs incompatible with this process are:
- Tetracyclines (Minocycline, Tetracycline, Doxycycline). They negatively affect the development of bone tissue and have a toxic effect on the baby’s systems and organs.
- Lincosamides (Lincomycin). They can negatively affect the intestinal microflora, leading to diarrhea and thrush; may damage the mucous membrane and cause bleeding.
- Fluoroquinolones (Ciprofloxacin, Tsiprolet, Norfloxacin and others). They should be avoided due to the theoretical risk of arthropathy.
- Sulfonamides (Biseptol, Sulfacyl sodium). They have a toxic effect on the organs and tissues of the baby, in particular, they can disrupt the functioning of the liver. They are best avoided in infants with hyperbilirubinemia or glucose-6-phosphate dehydrogenase deficiency.
- Aminoglycosides (Gentamicin, Netromycin). The instructions for use say that when taking this drug, breastfeeding should be interrupted - and for good reason. Despite the fact that they pass into breast milk in small quantities, even so they can have a toxic effect on the child, affecting the kidneys, organs of vision and hearing.
Approved antibiotics for breastfeeding.
Always contact a competent specialist and do not self-medicate. You should not listen to the advice of a neighbor or friend who took some medications - these people will not be responsible for the consequences of their use!
Among the drugs of choice:
Macrolides (Azithromycin, Clarithromycin).
They are considered safe, but changes in intestinal flora and diarrhea in a child are possible. It is not recommended to take these medications in the first month after the baby is born.
Penicillins (Amoxicillin, Flemoxin solutab).
Considered safe. Note: Although the amoxicillin/clavulanic acid combination is widely used during lactation, there are no published data on the safety of clavulanic acid.
Cephalosporins (Ceftriaxin, Cefipime).
Considered relatively safe, due to low transfer into milk. However, third-generation cephalosporins have greater potential for altering intestinal flora.
The benefit of taking the medicine for the mother should be greater than the harm it will cause to the child. That is, you should not take an antibiotic while breastfeeding “just in case” or for prevention.
How to choose NSAIDs when breastfeeding
In order to determine whether women who are breastfeeding can take the drug, doctors at the Yusupov Hospital pay attention to the following factors:
- toxicity of the drug;
- how much of the drug enters the blood and breast milk;
- how quickly the drug is eliminated from the body (NSAIDs are optimal for a nursing mother, as they are completely neutralized within four hours);
- How quickly does the NSAID begin to act?
- consequences of overdose;
- side effects and contraindications;
- effect on breast milk, compatibility with breastfeeding.
NSAIDs to which the child is allergic should not be used during breastfeeding. Before using non-steroidal anti-inflammatory drugs, you should consult a pediatrician. Even if NSAIDs can be taken while breastfeeding, only a doctor will select the optimal dose of the drug depending on the individual characteristics of the baby’s development and the severity of the mother’s illness.
Rules for taking antibiotics.
- Monitor your child's reaction to your antibiotics. If loose stools, vomiting, rashes on the skin and mucous membranes appear, consult a doctor to adjust treatment.
- Strictly follow the grams of the drug - reducing the dose will only harm you, and the medicine will still get into the milk.
- Try to drink the antibiotic immediately after feeding - this will give you some time before the next one so that the concentration of the substance in the blood decreases.
- Take the tablet with plenty of water - this will dissolve it better and start working faster.
- If you are taking a group of drugs and interrupting breastfeeding, pay attention to the time it takes for the antibiotic to be removed from the body - for some it takes 1-2 days, for others it will take 6-7 days! Don't stop pumping and drink more clean water.
Attention: the article is for informational purposes only. For all questions, always consult only a specialist; do not trust the opinions of readers of forums on the Internet.
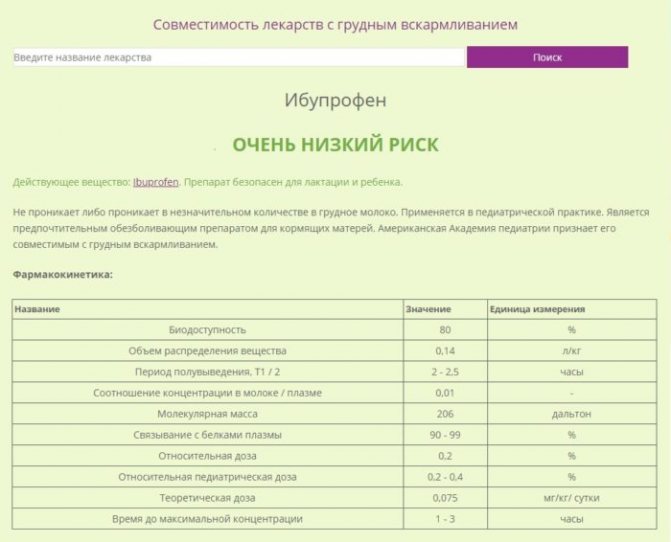
Safe NSAIDs during breastfeeding
Breastfeeding women can take ibuprofen (nurofen) for muscle, joint, headache and toothache, to reduce body temperature, 200-400 mg twice a day. The daily intake should not exceed 800 mg. Up to 0.7% of the drug gets into the milk, which is safe for the baby. Ketanov relieves pain and fever. The drug is not recommended for use within 21 days after birth. A single dose is 10 mg. The drug can be taken 3-4 times a day.
The safest NSAID for breastfeeding (breastfeeding) is diclofenac. The drug is not recommended for use by women suffering from arterial hypertension or gastric ulcers. The average therapeutic single dose is 25-50 mg. Diclofenac can be taken up to three times a day when breastfeeding.
The optimal NSAID during breastfeeding is paracetamol. The drug effectively reduces body temperature and reduces headaches. It is not effective for toothache or abdominal pain. 1% of the main active ingredient gets into milk, so the drug does not have a negative effect on nursing mothers and breastfed babies.
Paracetamol is a completely safe NSAID, since after 2 hours most of the drug is eliminated from the mother’s body, and after 4 hours it is completely neutralized. Breastfeeding mothers can take 500 mg of paracetamol 3 times a day, at least 4 hours apart. It is recommended to take the tablets after breastfeeding and no more than three days in a row. Paracetamol analogues are efferalgan and panadol.










