Causes of wounds
You can suspect the presence of small cracks if:
- the woman is in pain throughout the feeding;
- between applications, a burning sensation is felt in the nipple area;
- When you blot the nipple with a clean napkin, traces of blood remain on it.
Large cracks look like deep, even scratches and are very painful. Cracks in the nipples during feeding occur for the following reasons:
- improper latching on the breast by the baby;
- feeding technique is impaired;
- incorrect pumping tactics;
- improperly organized breast care;
- sensitive nipples;
- fungal and bacterial diseases of the skin of the nipple;
- problems with the vessels of the areola.
Let's talk in more detail about why nipple cracks appear.
Incorrect chest grip
Cracks appear if:
- when feeding, the baby grasps only the nipple;
- asymmetrical grip, when the child takes the nipple and areola from only one side of the breast;
- the latch may be initially correct, but during feeding, only the nipple ends up in the baby’s mouth;
- The baby cannot breastfeed effectively due to a short frenulum or neurological problems.
Violation of feeding technique
A nursing mother makes the following mistakes:
- Uncomfortable position for feeding. The baby's mouth should be directly at the nipple, the baby should not reach for the breast or turn his head. In this case, the woman puts the baby to her chest, and does not reach for him with her breasts. In other cases, the nipple rubs and cracks appear.
- Incorrect completion of feeding. The World Health Association recommends keeping your baby at the breast for as long as he needs. The mother must wait until the baby is full and lets go of the breast. If it becomes necessary to remove the breast, you need to insert a clean finger into the corner of the mouth of the sucking baby and turn it, the vacuum will be broken, and the nipple can be removed without injury.
- Use of pacifiers and pacifiers. The baby suckles on these devices in a completely different way than the breast. When alternating between nipple, bottle and pacifier, the baby gets confused and takes the breast incorrectly, resulting in abrasions and cracks.
Incorrect pumping
Typically, nipple problems when expressing occur when using a breast pump. A nozzle that is too large or too small will cause cracks. It is also necessary to regulate the intensity of operation of the device and promptly and thoroughly disinfect it to avoid infection. When manually expressing your breasts, it is difficult to develop cracks, because in this case the woman is guided by her sensations.
Breast skin care
Sensitive nipples
If the sensitive skin of the areola is the only reason for the appearance of cracks during feeding, then they go away on their own after the epidermis of the nipple is renewed. The skin becomes rougher, “gets used” to constant stress and the wounds heal.
Nipple skin diseases
Common pathogens that cause cracked nipples during breastfeeding are candida (a fungus that causes thrush) and staphylococcus (a bacteria). If such a problem occurs, treatment is prescribed by a doctor.
Vascular problems (vasospasm)
This is a spasm of the nipple vessels, which usually occurs after feeding. The woman feels a burning pain, both or one nipple turns white and becomes tense. This state lasts about a minute. Dry warmth on the chest - an ironed diaper, a heating pad wrapped in a towel - helps to alleviate suffering.
Massage and hardening
Breast care also includes massage, contrast showers and special gymnastics. They improve blood circulation, prevent the formation of congestion, and reduce the risk of stretch marks.
Massage can be done not only as I mentioned above, but also during water procedures. Direct a gentle stream of warm water onto the nipples for a minute, slightly moving the watering can to the right and left.
A contrast shower helps strengthen your breasts and restore skin elasticity. Its duration is at least 5 minutes: first hot water, then cool. Do not direct the stream of water to one point, but move it in a clockwise circular motion around the chest. After a shower, dry your breasts with a soft towel - from the nipples to the armpits. Do not rub your nipples - this will not strengthen, but will injure the delicate skin.
If your breasts are small, avoid wearing a bra at night or wear a cotton top. And don’t forget to take air baths before bed, leaving your chest “in free flight” for 20-30 minutes.
Many mothers are interested in whether it is possible to go to the bathhouse while breastfeeding. Of course, you can if you follow certain rules. A moderate steam bath improves your mood and helps you take proper care of your breasts.
Feed your baby correctly
Remember! The lion's share of all problems with the skin of the nipples is the result of improper attachment of the child.
To prevent the appearance of cracks already in the maternity hospital, even before giving birth, try to learn more about breastfeeding. This can be done by visiting our section.
Choose several comfortable positions for feeding. When sucking, the baby's head, neck, and back should be in one line. Avoid tilting or turning your head. The positions should also be comfortable for the mother, because in the first few months feeding can last about an hour.
The first breastfeeding is very important. At the beginning of feeding, tickle the baby's cheek with your finger; the baby will instinctively open his mouth wide. Quickly place the nipple in your mouth so that the baby captures as much of the areola as possible. If you don't succeed the first time, pick up the breast (by inserting your finger into the corner of your mouth) and try again. If a mother immediately teaches her child to latch on to the breast correctly, this will save her from many problems in the future.
To avoid cracks, always monitor how feeding is going. Signs that your baby is breastfeeding correctly:
- The areola and nipple are in the baby's mouth. If the baby does not capture the entire areola, then its main part should be visible above the upper lip.
- The baby's mouth is wide open, lips turned outward. If the child turns his lips inward, but at the same time grabs the areola, and not just the nipple, you can gently straighten the tucked lip with your finger.
- Sometimes a tongue can be seen between the chest and lower lip.
- During feeding, the baby's chin is pressed against the mother's chest.
- When sucking, only gulps are heard. If you hear smacking during feeding, this means that the sucking vacuum has been broken. Take the breast and insert the nipple into the baby's mouth correctly.
- The chest empties well.
- It is normal to experience pain when starting to feed in the first few weeks. The discomfort goes away after a couple of minutes. If the pain accompanies the entire feeding and intensifies, it is possible that cracks have already appeared on the nipple.
If the latch becomes incorrect during feeding, remove the breast from the baby and reattach it. The baby will soon learn to take the nipple properly.
If a mother is not confident in her breastfeeding technique, it makes sense to consult a doctor or invite a competent breastfeeding consultant. If it is not possible to urgently call help at home, consultants can give preliminary advice in absentia on eliminating the causes of cracked nipples during feeding; they will take photos of the pose and grip on the Internet.
Why is lactostasis dangerous?
Many breastfeeding women do not pay any attention to the appearance of painful areas in the mammary glands, believing that the baby will be able to “dissolve” the problematic part of the mammary gland, ridding it of milk. This is only true to some extent. Colostrum, like transitional milk, has a fairly thick consistency; if the outflow of milk is difficult for some reason, it becomes even thicker, making it much more difficult for the baby to suck. The baby sucks out more liquid milk from neighboring areas, and the problem area remains practically untouched. Milk is pyrogenic, meaning that the accumulation of milk can cause a high fever. With lactostasis, this temperature can reach significant numbers ( in some cases, up to 40 degrees Celsius
).
This is exactly the condition that is described by the popular expression “ the milk in the breast is burning
.” Typically, such an increase in temperature is very difficult to correct with medication. Here the only and effective method of treatment is to free the problematic mammary gland from milk - “drain the breast.”
Read more What to do when it hurts to write
In the maternity hospital, the “decantation” procedure is carried out by obstetricians, this is due to the fact that the young mother ( especially the first-time mother)
), most often, does not have sufficient practical skills to independently carry out this manipulation. If the baby sucks at the breast sluggishly and a lot of milk is produced, decantation must be done several times in order to expand the milk ducts and, thereby, facilitate the outflow of milk from the mammary glands. The first decantation procedure, usually performed on days 3–4, can be painful, but later the pain becomes less. The number of these procedures for each breastfeeding woman may be different; for some, one decantation is enough, for others, 2–3 are needed.
After discharge from the maternity hospital, there will no longer be a constant opportunity to turn to a midwife for help. Therefore, it is advisable to take the phone number of the health worker you like in order to, as a last resort, call a midwife at home. At home, you also need to constantly monitor the condition of the mammary glands. If the baby sucks weakly, or you have a lot of milk, excess milk from the mammary gland from which you fed the baby needs to be expressed. You can do this with your hands, but it is much more convenient to express milk using a breast pump.
Currently, there are many models of breast pumps, and their prices sometimes differ significantly. Choosing the optimal breast pump for each specific case is quite difficult. Sometimes you have to try different options. If you have friends who recently bought a breast pump and used it, you can take the breast pump from them “for testing” ( before use, parts of the breast pump that come into contact with the mammary gland or milk must be sterilized
). Remember, no matter what breast pump you choose, when working with it, you must massage the expressed mammary gland in a circular motion, as if directing milk from various sectors of the mammary gland to the nipple. Only in this case will the breast pump be able to cope with its task; without massage, even the most expensive model may turn out to be useless.
At the first symptoms of milk stagnation ( the appearance of painful areas on one or both mammary glands, increased body temperature, swelling of the mammary gland or the appearance of hardening in it
) you need to pump your breasts yourself using the same movements as the midwife did. Remember, you must massage the mammary gland in a circle and only towards the nipple, and not vice versa. If you feel that you cannot cope on your own, seek help from a midwife. The most dangerous complication of lactostasis is the development of mastitis.
How to prevent the formation of cracks?
Feeding a baby with a cracked nipple is painful, and treatment takes some time. It is much easier to pay attention to the prevention of this unpleasant problem. Contrary to popular belief, no amount of “preparing” your nipples for breastfeeding during pregnancy will reduce your chances of developing cracks. Rubbing with a rough towel can damage the delicate skin of the breast and contribute to injury.
If a woman has flat or inverted nipples, it is useless to “stretch” them yourself. A properly attached baby will give them the desired shape within a few feedings. Women with problem nipples need to pay special attention to the correct grip of the breast, as they are at risk of injury to the skin of the areola.
You need to monitor your latch from the very first feeding.
Properly organized care for the skin of the breast and nipple also helps to avoid cracks. There is no need to wash your breasts before each feeding, just rinse them once a day. Use soaps and gels less often so as not to dry out the nipple skin.
The underwear should provide good support for the breasts between feedings. Give preference to models made of natural fabric, without wires, and with wide straps. If your milk leaks between feedings, use special breast pads in your bra cups.
After feeding, squeeze a drop of milk from each gland, spread over the nipples and allow to air dry. This helps prevent various infections and prevents the appearance of cracks. Dry nipple skin can be lubricated with vegetable oil, such as olive oil, after feeding.
Don't allow stagnation!
In the first week after giving birth, do not drink a lot of water so as not to stimulate milk production. Also learn everything about foods that increase breast milk lactation, and try to eliminate them from your diet for a while. A newborn will not be able to suck out excessive amounts of milk completely, which means stagnation is quite possible.
With lactostasis, the breasts become very swollen and painful, lumps appear, and the temperature rises. Stagnation is dangerous because it creates a favorable environment for pathogens, not to mention terrible discomfort and the development of mastitis.

Prevention of stagnation is elementary:
- if the baby has not sucked all the milk, be sure to express (manually or with a breast pump);
- Massage your breasts with light circular movements after each feeding (pumping);
- apply to the breast, leaving the nipple open, compresses - honey, beetroot, cottage cheese - they can be made quickly according to folk recipes, but it is still better to use only for prevention, and in case of serious problems, be sure to consult a doctor.
Treatment of cracked nipples
If you notice cracks in your nipples during feeding, what should you do first? First you need to determine the cause of the cracks. Evaluate the appearance of the nipple (with thrush a white coating appears on it), the correctness of the latch. Think about how feedings are organized. When the causes are established, begin to eliminate them and remember: nipple cracks will not heal until all negative factors are corrected.
See also my video tutorial about cracks on the chest:
Moms are often given advice that they really don’t need to implement when dealing with cracked nipples:
- Stop breastfeeding. If it is unbearably painful for a woman to feed, you can take a break of no more than 12 hours for each breast. During this time, you need to heal the cracks and actively take on correcting the incorrect organization of feeding.
- Feed your baby less often. At the next feeding, the baby will be hungry and will suck much more intensely, which means the process will be more painful and the nipples will be more injured. Best to continue.
- Feed the baby expressed milk. Expressing can make cracks worse.
- Feeding in pads. The exception is cases when the pain is unbearable. You can feed in the pad for one day until the wounds heal a little. In the breastplate, the breasts are difficult to empty. Read about this method of feeding in the article:.
- Lubricate the nipple cracks with iodine, brilliant green, and alcohol. These products will dry out the skin even more and make the problem worse.
Treatment of cracks involves the use of ointments, decoctions and creams. When the skin dries out or the first micro-wounds appear, your own milk will help you. After finishing feeding, lubricate the surface of the nipple with a drop and let it dry.
Important!
If there is noticeable pus in the wounds, redness, pain in the breast itself, or a rise in temperature, you should immediately consult a doctor.
If cracks appear on the nipples during feeding, it is better not to use traditional methods of treatment. Various decoctions and homemade ointments can cause more harm than good.
To treat cracks, purchase Solcoseryl gel at the pharmacy. Be careful: there are ointments and creams on sale, but you need the gel.
Small cracks can be treated independently, but deep wounds require an in-person consultation with a lactation consultant.
So, blow the nipple of the damaged breast with a hairdryer, the wound should be dry. Then, using a match or a toothpick, apply a small amount of gel inside the wound. The gel glues the wound and helps it heal faster. It is best to feed the damaged breast no more than once every 3 hours. This is a temporary measure. As soon as the wound heals, start feeding at your usual rhythm.
If, when putting the baby to the breast, the crack opens again and does not heal, you need to seek in-person help. If the baby is not applied correctly to the breast, the crack cannot be completely eliminated.
Purified Lanolin can be used to treat noticeable cracks. It seals the wound, preventing microorganisms from penetrating inside, and has a healing effect.
In addition, the substance blocks the nerve endings, and feeding will no longer be so painful.
Lanolin is a natural material and can remain on the breast during breastfeeding. Pharmacies offer a large number of creams and ointments for cracked nipples based on this active ingredient.
It is advisable to purchase pure lanolin, as additional components can cause allergies. The nipple should be constantly covered with the chosen product throughout the entire treatment period, even during feedings.
Solcoseryl ointment has a good healing effect, but it must be washed off before feeding.
Cracked nipples are an unpleasant problem that often leads to refusal of breastfeeding. There is no reason to deprive your baby of mother's milk and endure the inconvenience associated with switching to formula feeding. With a little effort, any woman can cope with this condition and continue to breastfeed her baby.
the Breastfeeding Mother's Nutrition GUIDE right now
to protect your baby from allergies, colic and abdominal pain.
Enter your email and click on the “GET” button
Various types of fungi constantly live on the human body, and only when the body’s defenses are reduced can they cause diseases. Thrush on the nipples is much more common than many people think. It does not always have a clear clinical picture; it is difficult to diagnose it in a timely and unambiguous manner. Most often, such conditions are interpreted as cracks associated with improper application.
Thrush of the areola and nipple does not go away without a trace even for the child. How to detect and treat the disease in time?
Gymnastic sketches
Special gymnastics for the chest will not take much time, but if you do it regularly, you will definitely notice the result.

Here are a few simple exercises from my complex:
- connect your palms to each other at chest level and alternately squeeze and unclench an invisible 100-dollar bill with them;
- place your hands on your waist and rise onto your toes, moving your elbows as far back as possible;
- stretch and hold a tight elastic band over your head for 10-15 seconds;
- do push-ups from everything you can - from a chair, window sill, table top, floor.
And for today I have all the advice. Tell us how you care for your breasts after feeding. Maybe I forgot to mention something? If the article was useful to you, share it with your friends on social networks. I say goodbye to new interesting topics, and for dessert, as usual, a useful video:
Signs of thrush
All women are familiar with a fungal infection of the vaginal mucosa with unpleasant discharge, itching and discomfort. The same kind of fungi can cause an infectious process on the surface of the areola and nipple.
Mom
Candidal lesions cannot always be clearly differentiated from other diseases and conditions. The main signs of what thrush on the nipples looks like can be described as follows:
Also, signs of thrush on a woman’s nipples can be combined with candidiasis of the vaginal mucosa, corners and oral cavity. This indicates a serious immunodeficiency condition.
The child has
You have to deal with diagnosing thrush in a baby more often. This is primarily due to a more vivid clinical picture. The main features are as follows:
- In most cases, the oral mucosa is affected. The mother immediately notices the appearance of a white coating on the baby’s tongue. It can be of varying degrees of severity - from minor spots to quite dense, covering the entire surface. When removing plaque from the tongue with a cotton-gauze swab, which is done without much difficulty, a bright red mucous membrane appears underneath it. The gums, palate, etc. can be affected in a similar way.
- Depending on the severity of thrush, the child may either not change his general condition or become whiny and refuse to eat (due to painful sucking).
- Another common localization of candidal lesions is the inguinal and axillary folds. In this case, most often the pathology appears in the form of small non-healing ulcers with a bright red surface. To prevent fold candidiasis, it is necessary to provide air baths to the baby.
Watch the video about thrush in the mouth of a baby:
Procedures to restore your previous shape
Having noticed the shape of your breasts after childbirth, you can independently begin to restore their previous forms, while it is better to use a set of techniques that are characterized by increased efficiency and effectiveness.
For this purpose, special masks and massage procedures are used, as well as a set of physical exercises and moderate loads that strengthen the muscles and restore their elasticity to the required level.

Self-prepared or purchased cosmetic masks will not make your breasts firm, but they will help you get rid of stretch marks or other skin defects and stop the appearance of wrinkles.

Using them in combination with exercises and massage will help restore your bust to an attractive and aesthetic appearance, without spending a lot of personal time and financial investments.

Massage exercises carried out independently are necessary to restore blood flow and increase the elasticity of the skin, but it is not necessary to contact a cosmetologist, following certain massage techniques:
- pressure and vibration;
- vacuum massage;
- lymphatic drainage massage;
- home cryotherapy.

Knowing how to tighten breasts after childbirth, it is necessary to include special exercises in the complex of procedures that will help to effectively and quickly restore the elasticity of muscles and connective tissue.
Possible reasons for the appearance
During pregnancy and after childbirth, all women experience. This is due to many reasons - from carrying half-alien genetic material to stress and blood loss.
All this leads to new mothers having problems and diseases that have never bothered her before. It is important to know and understand what is happening and how it can be prevented.
As a rule, nipple thrush occurs only during lactation. Along with this, damage to the vaginal mucosa or oral cavity is possible. This is due to the following factors:
- immunodeficiency, especially against the background of anemia or exacerbation of chronic diseases;
- increased humidity due to constant sucking;
- frequent cracks, especially in the first months of feeding;
- milk is a nutritional basis for the reproduction of pathogens.
The fact that women can take (for example, after a cesarean section or complicated childbirth) hormonal and some others, which reduce the body’s protective properties, also plays a role. Also, thrush on the nipples during breastfeeding often appears in girls with various metabolic disorders - obesity, diabetes, etc.
Breasts after childbirth: effective ways to restore beauty and tighten them (75 photos)
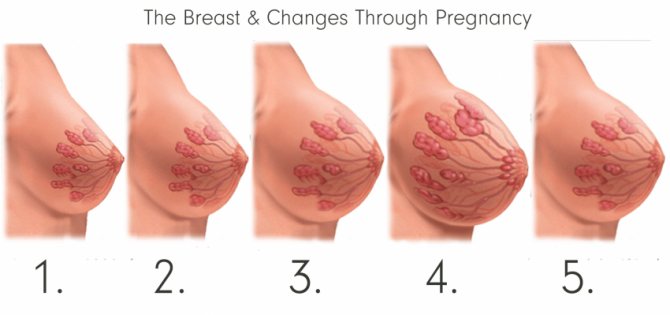
During pregnancy, every woman notices certain changes in her body, in addition to the enlarged belly, the breasts grow, which are necessary for breastfeeding the baby. If your breasts hurt after childbirth and a burning sensation is felt in the area of the mammary glands, it means that the lactation period is proceeding normally and the child will be provided with food at the beginning of his life.

Many women note that in the postpartum period, the breasts again change their shape and the lush bust sags, losing elasticity due to weakening of the muscles and ligaments, which is most frustrating for young mothers.
After the end of lactation, you can begin to correct the situation; for this you can use various methods that differ in effectiveness, but help you feel young and attractive again.

The effect of thrush on breastfeeding
The degree of influence of thrush on the intensity of breastfeeding depends on its clinical manifestations in the mother and baby. We have to talk about changes in lactation when the oral mucosa is damaged in a child.
So, if thrush causes pain to the baby, he will refuse breastfeeding or even artificial feeding for obvious reasons. At the same time, the rest of the time he will also behave restlessly, as he will be hungry.
If the severity of thrush is insignificant, and it does not bring any unpleasant sensations to the baby, then you may not notice any changes in the intensity of sucking.
If the mother has thrush and her nipples hurt, the woman will try to reduce the feeding time. This will also negatively affect the child’s mood, causing him to ask for food more often.
As a result, thrush can lead to either a slight decrease in lactation or its complete cessation. Therefore, it is important to promptly identify and treat the pathology.
Hygiene measures
You should always wash your hands well with soap first. Before each feeding, the breasts are washed with warm water. You need to wash it with soap no more than 1-2 times a day. Also, do not wipe the skin with alcohol or other disinfectant solutions. Regular baby soap is sufficient.
Breast massage is very useful for improving lactation and preventing milk stagnation. It, to one degree or another, always precedes feeding or pumping. The hand supporting the chest acts in a similar way. The gland tissue should be of the same density. If you feel areas of compaction, then in these places the massage should be more intense, but the emphasis should be on increasing not the strength, but the time of the massage. Eliminating compactions in the gland is an effective prevention of its inflammation (mastitis). It’s good to involve dad in this event.
Methods to combat thrush
To effectively combat thrush, in addition to basic treatment, it is necessary to follow some hygiene and lifestyle recommendations. These include:
- It is important to remember that warmth and moisture are the best conditions for fungal growth. Therefore, it is better to replace all synthetic underwear with cotton. If a woman uses special inserts to prevent milk leakage, they must be changed regularly, at least once an hour. But during treatment it is better not to use them at all.
- When using breast pumps, they must be thoroughly washed and boiled.
- Before each feeding, you should wash your hands, preferably using disposable towels.
- If a woman has other foci of candidal infection, it is also necessary to sanitize them. After all, their constant presence indicates immunodeficiency, and in such conditions it is impossible to cure the fungus.
- It is useful to additionally take bifidobacteria orally. They will gradually colonize the intestines, vagina and other mucous membranes, preventing the proliferation of pathogens.
- It is better to exclude thrush provoking foods from all foods. And this is sweet, salty, smoked, pickled, alcohol and plenty of spices.
- It is necessary to treat both mother and baby at the same time. Even despite the absence of manifestations in one person.
- If a woman practices freezing or expressing milk, then it is better to postpone this procedure during thrush.
Medicines
Treatment of nipple thrush is in many cases ineffective without the use of etiotropic therapy.
But it is better to select a remedy with a doctor, since many drugs are prohibited during breastfeeding.
Main medications used:
- Candida cream, based on the active ingredient clotrimazole, has multiple antifungal effects.
- Monistat or others similar. Here the active substance, miconazole, penetrates systemically in small quantities when used cutaneously.
- Nystatin ointment is a classic treatment option for thrush in children and adults, but it is less effective than other drugs.
- Pimafucin in the form of a cream can also be used to treat nipple thrush.
All formulations should be applied after feeding to prevent them from reaching the baby. To treat it, it is better to use traditional methods, and if significant changes occur, you should consult a doctor. Depending on the clinical picture, he will prescribe either topical or oral medications. “Candide” is a popular solution for treating the oral cavity, as well as nystatin drops orally.
Traditional methods
One of the well-known folk methods of combating thrush is treating the nipples and oral mucosa with a soda solution. To prepare it, you need to mix a teaspoon of soda in 150 - 200 ml of warm water. After that, frequently wipe the nipples and the child’s oral cavity with a cotton-gauze swab.
Thrush of any localization is the main sign of immunodeficiency. Therefore, candidal colpitis never appears in healthy women without any chronic diseases. In any case, it is easier and safer to prevent pathology than to treat it. Basic recommendations:
- Wet cleaning and ventilation of residential premises should be carried out regularly.
- It is useful to harden yourself and spend time in the “safe” sun.
- Linen should be washed at a temperature not lower than 60 degrees.
- It is advisable, especially for children, to wear all clothes made from natural fabrics.
- Proper nutrition, including a sufficient amount of fermented milk products, and regular physical activity are important for maintaining the health of mother and baby.
Many women doubt whether there can be thrush on the nipples. Even doctors do not always diagnose this condition on time and correctly. Therefore, candidiasis should be prevented before pregnancy.
And if any complaints arise from the mother or baby, you can always use safe folk methods. If the situation worsens, the child becomes restless and refuses to eat, you should seek medical help.
A small child, due to an incompletely formed immune system and reduced protective function of the mucous membranes, is very susceptible to the effects of pathogenic bacteria. They enter the baby's body mainly through the mouth. Therefore, any infection that occurs on the nipples during feeding immediately reaches the baby and can cause various diseases. In this regard, the mammary glands must be kept clean during breastfeeding.
In breast care, much attention should be paid to three factors:
- the right bra for nursing mothers,
- proper breast hygiene,
- use of breastfeeding accessories.
Breast care: choosing underwear for nursing mothers
During lactation, the mammary glands fill with milk, increase in size and become heavy. To prevent the vessels from being squeezed and the outflow of milk being disrupted, breast support is necessary. Therefore, during breastfeeding, nursing women are advised to wear a special nursing bra.
What to look for when choosing nursing underwear?
- A nursing bra should be made from natural fabrics. In this case, it will not cause allergies, will absorb moisture well and is easy to wash.
- Pay attention to the sensations. A nursing bra should provide good support. A small model will put pressure on the breast during milk flow and interfere with blood circulation. A bra that is too large can cause stretch marks and sagging breasts.
- For breastfeeding, it is recommended to choose a “wireless” bra, since when the breasts are full, they can put pressure on the breasts and cause stagnation of milk.
- The straps should be wide, which will evenly support the mammary glands.
- It is recommended to choose nursing bra models made from seamless material. If there are seams on the product, they should not pass through the area of the areola and nipple, so as not to rub them and cause irritation. During feeding, you will have to give up lace models: they can rub the sensitive skin around the nipple.
- Bras for nursing mothers with a detachable upper part of the cup are very comfortable (you don’t have to remove it every time during feeding).
How many bras will you need?
After childbirth, a nursing mother's breasts are vulnerable to pathogens, so clean underwear is of particular importance. It is recommended to have at least two nursing bras and wash them regularly. At first (during the formation of lactation), due to possible leakage of milk, it is recommended to change them every day.
Breast care: clean and dry!
The basic rule of hygiene that every nursing mother should know is this: the breasts should always be clean and dry.
More recently, medical staff at maternity hospitals insisted that a nursing mother must wash her breasts before and after each feeding of the baby. However, this rule is outdated. Breastfeeding experts say that it is enough to wash your breasts 1-2 times a day while taking a shower. The fact is that when washing the breast, especially with soap, a protective layer of fat is removed from the skin of the areola and nipple, which contains special substances that prevent “harmful” microbes from penetrating the skin of the breast. In addition, frequent breast washing leads to dry skin and cracked nipples.
After a shower, your breasts should be gently blotted with a soft cloth. It is not recommended to rub it with a towel so as not to irritate the nipples during feeding.
After feeding, it is advisable to lubricate the nipples with drops of hind milk (the portion that is released at the end of feeding), as it has protective and healing properties, protecting the skin from dryness.
If the mother’s skin is very sensitive, then to prevent cracks you can use a special nipple cream during breastfeeding. Immediately after feeding, it should be applied to the nipple and areola in a thin layer. There are creams that do not need to be washed off before the next feeding; they are completely safe for the baby. It is clear that they are much more convenient to use.
After feeding and between them, it is necessary to arrange air baths for the breast, i.e. keep it open for about 10 minutes. After each feeding, the nipple should be allowed to air dry on its own.
Under no circumstances should you use various disinfectants (brilliant, vodka, chlorophyllipt, alcohol, etc.) to treat the nipple and areola. They dry out the skin of the nipple and areola, which causes cracks to form.
Breast accessories that will make your life easier:
Breast pads
Breast pads are disposable and reusable
. It is important that the nursing pad has a breathable surface and is waterproof. In addition, such inserts should absorb milk well, be soft, thin and pleasant when touching the breast.
Reusable nursing pads are made from natural cotton. They have less absorbency than disposable pads, so they have to be changed more often. These pads can be washed and reused. You can wash them by hand with baby soap or baby laundry detergent, or in the washing machine by selecting the gentle wash program. After washing, they must be rinsed well.
Disposable bra pads have 4 layers. The outer surface is breathable and waterproof. Inside the liner there is a soft absorbent pad and a dense layer of adsorbent. This way, the inner layer in contact with the skin remains dry, which reduces the risk of nipple inflammation.
Most disposable bra pads have a non-slip tape to prevent them from shifting around in the bra. It is important to change the inserts regularly (when they get wet), since, filled with milk, they become a good breeding ground for bacteria. In addition, their ability to absorb milk has its limit, after which they do not guarantee dryness. If the breast remains wet for a long time, this can cause cracks and infection of the mammary gland.
Pads for collecting leaking milk
There are also special pads to collect leaking breast milk. They are convenient for nursing mothers to use during hyperlactation, when there is too much milk in the breast. Externally, this device looks like a plastic “cup” that is inserted into the bra. One part of it is made of plastic, the other of silicone with a hole for the nipple. The nipple itself does not touch the surface of the pad due to the presence of a double bottom. To prevent nipple problems due to increased humidity, it is recommended to remove the shields every 2-3 hours and provide air baths for the breasts. After use, they must be washed and stored in a clean, closed container.
IMPORTANT!
Breastfeeding should not be accompanied by feelings of pain and discomfort. If these or other signs of trouble appear, the woman should carefully examine the mammary glands for swelling, redness, cracks and irritation. If any changes are detected, you should consult a doctor in order to eliminate the cause that is interfering with breastfeeding as quickly as possible.
Breast hygiene
Daily breast massage and taking a contrast shower will help improve blood circulation in the mammary glands and avoid stretch marks. Massage your breasts with water jets in a clockwise motion with warm and cool water alternately. After taking a shower, wipe your breasts with a towel using movements from the nipple to the armpit. Wear special supportive tops at night.
To keep your mammary glands in shape, do special exercises to strengthen your breasts. Here are some exercises. Repeat each at least 20 times.
- Clasp your hands in front of your chest, palms facing each other, as if in supplication. Squeeze your palms tightly for a few seconds, then release.
- Stand up straight, place your hands on your waist. As you rise onto your toes, move your elbows back as far as possible.
- Take an expander or a tight, wide elastic band about 50 cm long. Raise your arms above your head, stretch the elastic band, and hold it taut for ten seconds.
- Push-ups (from the floor or a chair) also help strengthen the muscles that support the chest.










