How does lactation develop?
Various methods are used to restore feeding.
The most common technique is the use of special nutrition to increase lactation. It consists of a dry milk mixture that is easily absorbed by the mother's body. This diet helps the glands work more actively. The mixture does not contain allergic substances. For this reason, treatment does not require giving up natural feeding. The feeding procedure itself should also be carried out correctly. Lactation should be carried out in a sitting position. It is also allowed to feed the baby lying on one side. The baby should be put to the breast at least 6 times a day. If the volume of milk does not increase, it is necessary to distribute the night time. Lack of milk can be determined by the child’s behavior and physiological processes.
If the baby is not full, the following signs occur:
- rare urination;
- anxiety and restlessness;
- reflex movement of the lips outside of feeding.
Many mothers do not know that the amount of milk can be determined by the number of times the baby urinates. On average, a newborn should empty the bladder at least 6 times a day. If the number of urinations is less, then the child does not have enough nutrition. It is necessary to increase the number of breastfeeding or introduce artificial nutrition.
You should also monitor the general condition of the child. After the next feeding, a well-fed baby can play or sleep peacefully. A hungry child is exposed to stress. He begins to worry, fidget, and refuses to sleep. In some cases, a sucking movement of the lips is observed. You should not take away the empty breast from such a baby.
Milk can come in even if you control your diet. Lactation is facilitated by the exclusion of fatty and fried foods from the diet. It is also necessary to avoid excessive consumption of salt, sugar and coffee. All these products cause fluid stagnation in the body. Lymph prevents the glands from functioning normally. Against this background, the milk came late or did not appear at all.
After a caesarean section, a woman should pay close attention to her health. If for some reason the patient’s milk does not come in, you should consult a specialist. Only a doctor can correctly determine the reasons for the lack of lactation and choose the safest method for restoring it. It is not recommended to solve the problem yourself. This can lead to mastitis and other complications.
Scientists have long proven that the amount of breast milk directly depends on the frequency of the baby’s attachment to the breast. It is better to do this immediately after birth - this way lactation will normalize faster.
Problem #1: early application
For the successful establishment of lactation, early latching of the baby to the breast plays an important role. In addition to the fact that the mother’s touch immediately after the birth of the baby, skin-to-skin contact can alleviate postpartum stress and facilitate the baby’s adaptation to a new world, early breastfeeding has a beneficial effect on the lactation process. Stimulation of the nipples causes a hormonal surge, which triggers the process of milk production.
During a natural birth, the baby's first breastfeeding should occur immediately after the baby is born or within the first 30 minutes after his birth. When the baby is born and makes its first cry, the doctor cuts the umbilical cord and places it on the mother's chest, helping him find and latch on to the nipple.
The possibility of early breastfeeding after a caesarean section depends on the type of anesthesia used and the well-being of the mother and child. With epidural anesthesia (an anesthetic is injected into the membranes of the spinal cord and the mother is conscious during the operation), the baby can be put to the breast immediately after birth without waiting for the end of the operation.
During general anesthesia, when the mother is still under the influence of anesthesia and anesthetic after the birth of the baby, it is impossible to put the baby to the breast. The first breastfeeding after a cesarean section is most often carried out after the woman has recovered from anesthesia and been transferred to the postoperative ward, and often it can be postponed until the woman is transferred to the postpartum ward. It often happens that the baby is brought to his mother, but he refuses to suckle.
MORE ABOUT: ✅ What are the benefits of a stalk of celery for women -
This is because the birth process itself is different for caesarean section babies. There is no phase of the baby passing through the birth canal, which prepares it for entering another environment. Caesarean babies require more time to adapt to new living conditions and overcome postpartum stress.
Thus, babies born naturally “come to their senses” 15–30 minutes after birth, and babies after a cesarean section need 1.5–2 hours. And all this time the baby will behave sluggishly, not feeling the desire to attach to his mother’s breast.
As numerous studies show, Caesar calves begin to show sucking activity within the first six hours after birth. And it is during this time period that the baby must be put to the breast for the first time.
If the baby's sucking activity is low or absent, it is necessary to offer him the breast for every concern until he begins to suck actively.
Breastfeeding after caesarean section: when milk comes in normally, why not
Breastfeeding after a cesarean section can begin after suturing the anterior abdominal wall, if the mother is conscious. Lactation is stimulated by putting the baby to the breast and irritating the receptors, as well as the onset of contractions during childbirth.
During the natural process of labor, this stimulates the production of colostrum, and breast milk returns to normal within 2-4 days. During a caesarean section, this process may be delayed, and colostrum appears only after a day, and full milk within a week.
If the operation was planned, then contractions occur one way or another, which is the impetus for the onset of lactation. But if the indications for surgery arose earlier than the expected due date, this may lead to a delay in the mother’s lactation.
The beginning of feeding also depends on the anesthesia that the woman in labor received: after general anesthesia, it takes about 5-6 hours for the woman to regain consciousness and be able to feed the baby. After regional anesthesia, breastfeeding can begin immediately after birth.
The first to appear is thick colostrum, which differs in composition from breast milk and contains more protein compared to milk; the process of its production will also be affected by the condition of the mother’s body.
| Problem | Causes | Mechanism |
| No colostrum |
| Metabolic and hormonal disorders due to these reasons lead to the impossibility of colostrum formation due to the toxic effects of metabolites, insufficient protein content; in case of decompensated pathologies of other organs and systems, the survival of the organism is dominant, which leads to delayed lactation after surgery |
| The baby does not latch on to the breast |
| The child's serious condition and congenital anomalies disrupt the development of the nervous system and affect the sucking reflex. This is also facilitated by the very fact of operative delivery. Using a pacifier instead of a breast is much easier, so the baby will not want to put in the effort to start feeding on his own |
| Mother cannot start breastfeeding |
| The mother cannot breastfeed in an unconscious state, with depression of the nervous system |
Another problem after a cesarean section can be postpartum depression, which suppresses all instincts to care for the child. However, refusal to breastfeed may be an early and first symptom.

Also, the arrival of milk is facilitated by a positive attitude and peace of mind of the mother: anxiety, lack of help and support from loved ones can make breastfeeding impossible.
After a caesarean section, the baby is delivered almost immediately if the mother is in a stable condition. If she goes to intensive care, she will see the baby in 1-3 days, depending on her condition. The same applies to resuscitation for a child; only after stabilization will he be returned to his mother for care and feeding.
Sometimes antibiotics may be required after a caesarean section, which may affect breastfeeding. Antibiotics pass into breast milk and can cause unwanted reactions in the baby, so not all drugs are allowed to be prescribed.
If, due to vital necessity, the mother must take drugs prohibited during feeding, then during this period and until the drug is completely eliminated, she cannot feed the baby with her milk, and the baby is transferred to artificial feeding.
| Allowed | Prohibited or no data |
|
|
When breastfeeding, restrictions also apply to painkillers.
| Allowed | Prohibited |
|
|
Medicines should be taken according to the following rules:
- observe dosages;
- do not use for more than three days;
- if the course is ineffective, immediately consult a doctor;
- do not combine several drugs;
- take tablets after feeding.
In the first days after cesarean section, while breastfeeding, you can not eat everything, so as not to increase the risk of complications for the mother and child. On the first day after surgery, it is not advisable to eat anything; you can drink water with lemon. On the second day, low-fat chicken broth without vegetables, meat and salt is allowed, 150-200 ml 2-3 times a day. You can also eat something fermented milk: kefir, etc. It is undesirable to use sweet and fruit additives.
On the third day the diet is supplemented with:
- mashed porridge;
- cottage cheese casseroles;
- steam cutlets;
- meat soufflé;
- rosehip or compote.
Products must be crushed and free of preservatives. If a woman has problems with stool, then the diet is subsequently supplemented with strengthening or laxative components. In the first week, the mother is allowed to eat almost everything recommended for breastfeeding:
- low-fat steamed meat dishes;
- soups and broths;
- cottage cheese dishes;
- cereals in water or milk half and half with water;
- boiled pasta;
- vegetables, preferably steamed with the gradual addition of fresh ones;
- baked apples;
- dairy products;
- bread and soft rolls.
Fresh fruits and vegetables can be added to the diet a week after surgery. Red-orange fruits should be avoided to avoid causing allergies, as well as strawberries and citrus fruits.
To maintain lactation, you should follow simple recommendations:
- correctly attach the baby to the breast upon request;
- carry out the prevention of lactostasis and treat all diseases in a timely manner;
- eat rationally with dietary restrictions;
- sleep at least 8-9 hours a day;
- avoid stress, infections, significant workload;
- maintain a positive emotional background;
- wear clothes made from natural fabrics and special underwear;
- monitor the condition of other organs and systems;
- walk in the fresh air with your child.
The optimal duration of breastfeeding is considered to be 1-1.5 years. At certain times, complementary foods should be introduced to transition the child to an adult diet and develop the jaw and facial skeleton. At this time, breastfeeding also continues, but to a lesser extent.
Often, even after resuscitation is a thing of the past, and you put the baby to the breast, the milk supply stops. The situation is standard, even if you complied with all the requirements and pumped regularly. Why is this happening? There are several reasons:
- Expressing is not as effective as sucking. However, it is this procedure that allows you to ensure a minimum when there is no milk at all.
- Milk comes within 9 days after surgery. If you have little natural food for your baby, there is no need to introduce formula feeding. A small volume is enough for the baby, especially in the first days of life.

The wet diaper test developed by WHO helps determine whether the baby is getting enough nutrition. What activities does it include? You should monitor how often your baby urinates. In the first two days of life, the amount should be two times daily, from the third day it increases to four, from the sixth to six.
When is supplementary feeding necessary? Its introduction is necessary in the following cases:
- The baby is premature. These little babies have an impaired sucking reflex; they cannot suck out enough milk on their own, so pumping and regular feeding are required.
- Your milk is not enough. If the wet diaper test fails, supplemental feeding must be introduced immediately. The child does not receive the necessary food, he is weakened, nervous, and cannot stimulate lactation. This leads to defective development, deviations, diseases, the baby does not sleep, and constantly wants to eat.

To stabilize feeding after a cesarean section, introduce supplementary feeding correctly. To do this, follow a few rules:
- Choose the right method. In the maternity hospital, they usually use bottles with nipples, but you should refuse them; use a spoon, pipette, or syringe if the child is in the same room with you.
- Be consistent. At the beginning of the procedure, put the baby to the breast, then feed him with a spoon or pipette, and complete the process with the same attachment.
- Volume is also important. Regardless of how much milk is produced, in the first 10 days of life you should not give more than 30 mg at a time. Exceeding the volume is also harmful; digestion and general well-being of the baby can be disrupted.
- Switch to natural feeding. A diaper test should be carried out once every three days; as soon as the number of urinations returns to normal, reduce the amount of supplementary feeding. If your milk is enough, you need to completely abandon formula.
Normalizing lactation after cesarean section is a hot topic for mothers who gave birth this way (more details in the article: the most useful products for lactation of a nursing mother). If you believe the reviews and recommendations of doctors, the problem is easy to solve. Just follow the established procedure, which will stabilize the situation within a week. With early supplementary feeding, the problem can be brought under control within two weeks.
First application after caesarean section
Everyone knows that the first time a baby is placed on the mother’s breast is of great importance for how breastfeeding will proceed in detail and how quickly the baby adapts to new conditions.
In addition, stimulation of the nipples, the mother’s emotions from the realization that she has put her baby to her breast for the first time - all this gives a powerful impetus to the body’s recovery mechanisms, uterine contractions and a signal to activate the production of breast milk.
If a woman had a caesarean section under regional anesthesia, then there should be no problems with the first application. Sometimes the baby is handed over to the mother immediately after extraction, even before the surgeon finishes stitching. This, of course, is the best option, since it is important for the baby to be in the caring hands of his mother: he will be in comfortable conditions and will take over his mother’s microflora, which is also important.
However, if the operation was complex and was performed under general anesthesia, then the woman may wake up only after a few hours.
There is no need to be upset about this. Even if the attachment did not take place in the first hour after birth, this does not mean at all that you can forget about breastfeeding after a cesarean section. Yes, it will be a little more difficult for you, but if you want to feed your baby milk, then you will overcome all difficulties. Try to provide the first feeding within 6 hours after the baby is born, as during this time he has a high sucking activity.
Judging impartially, almost all mothers who give birth in Russian maternity hospitals both naturally and by caesarean section put their baby to the breast for the first time for a few minutes, and ideally this should be at least half an hour for each breast. So, if the first attachment were the decisive factor, then natural feeding would practically never occur in our country.
Another important point is to agree with the staff or ask relatives to make sure that the baby does not receive any other food until you can provide him with a full hour-long breastfeeding, and ask him to bring the baby to you as soon as you can feed him.
If the baby managed to try feeding from the nipple before he was attached to his mother's breast, he may have some difficulty latching on to the nipple. Don't be afraid to help him, take the breast with your hand closer to the areola and try to place the nipple in the baby's mouth as deeply as possible.
Even those babies who immediately receive their mother’s breast sometimes have difficulty latching, so at first they need to be helped and taught how to grasp the nipple correctly. But when the child gets a little stronger and understands how tasty his mother’s milk is, he will not need help. You will even be surprised at how deftly he will learn to cope with this task - to suck his mother’s breast anywhere and in the most unexpected positions.
First, you need to completely stop using a pacifier. If the child is in the same room with you, this is not difficult. But if you can't see him all the time, try to convince the staff not to give the baby a bottle and check this yourself periodically.
Secondly, allow the baby to stay at the breast for as long as he needs. At first, the baby may get tired of sucking and take several breaks before he is full.
Premature and weakened babies need supplemental feeding because it is difficult for them to breastfeed for a long time and they often fall asleep exhausted or begin to worry without receiving the required amount of nutrition.
Supplementary feeding will help the baby gain strength, stop being nervous and suckle at the breast for as long as possible, stimulating the mother's milk production. For supplementary feeding, use a spoon or pipette and expressed milk.
Healthy but crying babies in the first days after birth, as a rule, do not need supplemental feeding. They cry from stress. You can calm such a child either by rocking him in your arms, or in no way - you just have to wait and let the baby cry.
Many mothers believe that the baby is hungry and feed him additional formula, after which the baby calmly falls asleep. However, most pediatricians and lactation consultants say that the baby does not suffer from hunger, but falls asleep after the formula because it is difficult to digest. You can determine whether your baby has enough nutrition by the number of urinations.
The minimum number of urinations in a child who does not suffer from hunger, and therefore does not need additional feeding:
- the first three days – 2;
- from the third to the sixth day - 4;
- further – at least 6.
Quite often, mothers are faced with the fact that the child gets used to feeding according to the schedule, cannot suckle at the breast in the correct position and simply cries.
The baby will literally have to be taught how to latch onto the breast correctly. At first he will most likely resist. Spit out the nipple and turn away from the breast. Don’t be upset, sooner or later the baby will want to eat and will reach out to you. You need to be patient a little for innate reflexes to take over the first experience of a child receiving a pacifier instead of his mother's breast.
At the end of the article you will find a video that very clearly demonstrates how to hold your baby correctly and ensure optimal latching.
But what to do with the regime when the baby eats only at certain hours and sleeps the rest of the time?
You need to pay close attention to your child, especially an hour and a half after he falls asleep. Usually, at this moment, children begin to smack their lips in search of their mother’s breasts. This is the ideal time to pick up your baby and offer him the breast, without having to wake him up for this.
Experienced lactation consultants say that during proper feeding, namely frequent and natural feeding, hereditary mechanisms are triggered and endorphins are released in the baby’s body. Therefore, even if the baby is capricious when trying to take the nipple unsuccessfully, he is not in a state of stress.
Restoration of lactation after surgery
The problem when there is no milk for a long time after a caesarean section worries many women. But waiting until the process of its production begins on its own is wrong. Already in the intensive care unit, it is important to put the baby to the breast and stimulate the production of colostrum. At first, it will be released drop by drop until the level of oxytocin and prolactin, the hormones responsible for milk production, begins to rise.
It is not always possible for a woman who has undergone such a complex operation as a caesarean section to immediately begin to establish natural feeding. Various circumstances can interfere with this, for example, being in different rooms with the baby, prescribing broad-spectrum antibiotics, placing the newborn in an incubator or connecting to an artificial respiration apparatus. It is important to overcome difficulties in order to give the baby the opportunity to feed on mother's milk, a valuable source of vitamins and minerals.
Antibacterial drugs are prescribed after cesarean section for prophylactic purposes to avoid the development of an inflammatory process in the uterus. Young mothers worry that medications will change the composition of the milk and harm the baby, but such fears are not always justified.
Firstly, a specialist prescribes antibiotics for medicinal purposes, so you cannot refuse injections or tablets on your own. And secondly, today there are a lot of drugs that pass into breast milk in small amounts, which will not harm the newborn and will not affect the lactation process.

In some cases, after a cesarean section, a woman may be prescribed antibiotics.
If the baby is weak and reflexes are inhibited, the first feeding can be postponed to 5-6 hours, but not later. Full attachment involves the newborn sucking on one breast and then the other for at least 15 minutes on each. The main condition is that the first thing that enters the child’s mouth should be the mother’s mammary gland. In no case should you use a pacifier or a rubber nipple; this point is important to discuss with doctors before the start of the cesarean operation.
With this approach, it will be possible to maintain lactation, even if the baby is not in the same room as the mother. You can ask the grandmother to be in the intensive care unit with the woman and help in caring for the baby (this is allowed in paid maternity hospitals).

In the event of a difficult birth after a caesarean section, the woman may be transferred to the intensive care unit
Lack of milk
What to do if a nursing mother has little milk after a cesarean section? First you need to make sure that the baby is really not eating enough - conduct a test developed by WHO. The number of urinations in the first two days is two times every day, on the third day it increases to four times, on the sixth – to six. Under such conditions, there is no need for complementary feeding.
If the mother really has little milk, it is important to try to establish lactation and start supplementary feeding. First, the baby is applied to the breast, then food is given from a syringe or spoon, and the process is completed by applying it to the breast again. Three days later, a diaper test is carried out and if the milk volume increases, supplementary feeding is abandoned.
When combining artificial and natural feeding, the volume of the formula is gradually reduced, replacing it with breast milk.

The transition from artificial feeding to natural feeding should be gradual.
Stagnation
During the operation, the water balance in the woman’s body is disrupted, and she needs to drink plenty of fluids. But excessive water consumption provokes increased lactation, the breasts swell, the milk ducts become clogged - stagnation occurs. When you are in the room with your baby, you need to apply it to the glands as often as possible; over time, lactation will stabilize and the blockage will go away.
When the baby is separated from the mother, ordinary lactostasis will turn into mastitis, so you need to pump every 1.5-2 hours before starting regular breastfeeding. Massage procedures are useful, and health workers will teach you how to express properly after kneading the hardened gland.
Antibiotics and lactation after cesarean section
After a cesarean section, a woman is prescribed a course of antibiotics to prevent complications from developing. Read more about what complications there are after cesarean section→
In this regard, many mothers fear that drugs can penetrate through milk into the baby’s body and harm him. There is no clear opinion on this issue; it must be considered individually, in the context of the policy and equipment of the maternity hospital, as well as the condition of the mother. In any case, you need to consult your doctor and, if necessary, ask him to choose the safest medicine possible.
It would also be useful to consult with an anesthesiologist so that he can clarify whether anesthetics enter the bloodstream.
Don’t be embarrassed to ask questions or ask the maternity hospital staff for anything. You have every right to quality service and to have your opinion taken into account. However, do not rush to create scandals if you fail to achieve what you want, because this may turn against you. There are many peaceful ways to influence the nurse caring for your baby, from asking politely to stimulating her interest with a gift.
In return, you can get the opportunity to feed your baby on demand, and the guarantee that he will never be introduced to a pacifier. In any case, remember that only serious complications, which are extremely rare, and the mother’s disinterest in this issue can interfere with breastfeeding after a caesarean section. Don't worry, be consistent in your actions - and you will succeed!
About 20-30% of children in Belarus are born by caesarean section. And most mothers face problems establishing breastfeeding. Many people don't succeed at all. For many, this is an absolute consequence: since it’s a caesarean, then you don’t have to think about full-fledged breastfeeding.

Photo source: aimg.sk
This is wrong. It is possible to breastfeed after surgery!
In the article I will try to highlight the main points that a mother needs to take into account if a planned caesarean section is on the horizon, and it is useful for all expectant mothers to read, since a caesarean section can also be an emergency.
How to improve lactation after cesarean section
To establish breastfeeding after a caesarean section, it is important to put the baby to the breast as early as possible. Even a few drops of colostrum will trigger the production of antibodies, populate the baby’s intestines with beneficial flora, and activate the immune system. Feeding should be done on demand to ensure stimulation of lactation.
The procedure should not cause pain or discomfort. It is better to ask the midwife to be present at the first sessions to learn how to pump correctly.
Correct posture is very important for full lactation and resorption of lumps if they have formed in the mammary gland. The best option after a caesarean section is to hand feed to relieve pressure on the abdomen. The baby's chin should point towards stagnation if lactation is intense. During attachment, the baby should grasp most of the areola so as not to damage the nipple and not provoke the development of mastitis.
Breast massage
How to increase the lactation of a nursing mother after a cesarean section using breast massage? The procedure is carried out immediately before latching - this will facilitate the outflow of milk, help the baby to attach to the breast more easily and suck out more liquid.
The massage is carried out by supporting the breast with one hand, and with the other making smooth movements from the periphery to the nipple. Before the session, you can slightly warm up the gland by applying a warm towel - this will enhance lactation.

To establish lactation after cesarean section, it is necessary to normalize the condition of mother and child and allow the earliest possible contact for the first feeding. The baby can be put to the breast immediately after the operation if the woman’s condition is satisfactory.
Next, you should help the mother with feeding, since she is prohibited from lifting weights and actively moving. The staff of the medical institution and the relatives of the mother in labor play a big role in this. But a woman cannot always start breastfeeding after a cesarean section.
After surgery, breastfeeding is not always done; breastfeeding is refused due to the danger to the life and health of the mother or child in the following cases:
- the mother has decompensated severe somatic pathologies;
- there were complications during the operation;
- Caesarean section was performed for emergency reasons;
- the mother suffers from infectious diseases;
- the mother has cancer;
- a woman or child has an acute inflammatory process;
- The baby is in serious condition, general weakness is expressed.
If the mother or child is in intensive care or intensive care, feeding can be done only after the condition of both has stabilized. In this case, the mother must express milk, and the child must be provided with the necessary nutrients parenterally to maintain vital functions in intensive care or with artificial formula if the mother’s milk is not suitable for feeding due to infection or is unavailable due to lack.
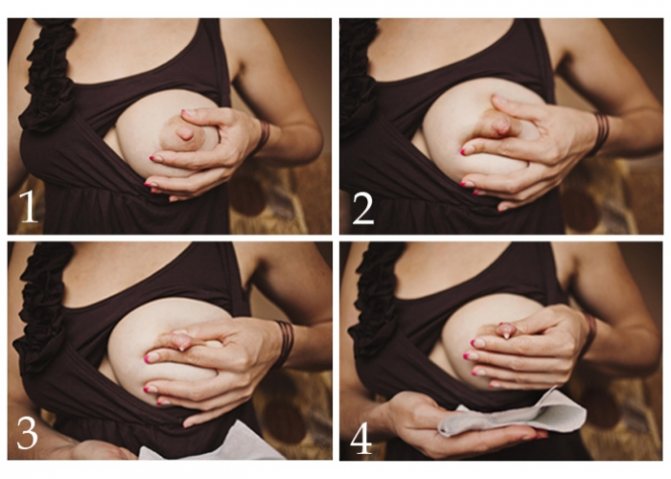
How to express milk correctly
The baby can be breastfed during a planned caesarean section after the abdominal cavity is closed, if the operation went well, the mother feels well and is able to carry out the first attachment with the help of doctors.
If there is a suspicion of infection, then feeding is postponed, as well as in case of pathologies in a newborn baby in case of severe weakness, prematurity and other serious diseases. For the first feeding, the baby and mother must be in a stable condition.
In order for breastfeeding to improve, you need to develop breast milk; for this, first of all, regular pumping is carried out if the baby does not latch on to the breast. This should be done with both glands every three hours, this helps reduce the risk of stagnation.
Gentle self-massage of the mammary glands also helps: with gentle circular movements, you should gently massage both breasts in turn, moving from the periphery to the nipple. Shower massage also helps in the future, when it is allowed: you need to massage each breast with jets of water in a circle for several minutes.
The best stimulation of lactation is feeding the baby, so you need to strive for its speedy onset: treat all diseases, follow medical recommendations. The mother’s diet is of great importance, as is her emotional mood: anxiety, lack of sleep and depression will contribute to a decrease in milk supply, while a positive attitude and sufficient rest will stimulate. You can also use medications prescribed by your doctor for this.
In the development of breast milk, a significant role is played by the general condition of the body, including hygienic measures: engorgement of the mammary glands, damage to the skin, and contamination should not be allowed. You need to wipe your breasts before and after each feeding and keep your skin clean.
For the lactation period, you should purchase special underwear made from natural materials, which will make feeding the baby easier. Do not wear tight clothing made from synthetic fibers.
If it is impossible to breastfeed your baby, you should express milk by hand, this must be done correctly so as not to harm the lactation process:
- sit comfortably, tune in to the upcoming process;
- drink warm tea the day before;
- gently stimulate the nipple with gentle movements;
- take a sterile milk container and place it under the breast with your left hand;
- clasp your chest with your right hand as follows: place your thumb on top at the border of the skin and areola, and the rest around the bottom;
- use gentle pressing circular movements to move from the periphery to the center;
- repeat movements until milk appears;
- express the breast for 5-7 minutes until emptying and repeat on the other side;
- Curl your fingers into a ring and relax when milk appears.
It is forbidden:
- apply more force until painful sensations appear;
- squeeze the nipples for a long time, you need to press on the area around the nipples, except in cases where it is necessary to “soften” the hardened nipples;
- lean forward;
- rub, knead or do something carelessly and carelessly, scratch the skin;
- squeeze out too much milk: to prevent stagnation, it is enough to express the breast not completely, but if you need to make a supply of milk, the process will be longer and more gentle.
To stimulate lactation with foods, you should follow dietary recommendations. Experts have calculated that for normal breastfeeding, a woman should increase her diet by no more than 500 kcal, but this must be done through a balanced diet: protein foods, vegetables, fruits. Increased lactation is promoted by:
- broths and soups from lean meats;
- cereal porridges (buckwheat, oatmeal, rice);
- vegetables and fruits;
- herbal teas;
- dairy products;
- lettuce, parsley, dill and other greens.
You should avoid fatty meats, fatty broths, and lamb. If a baby develops constipation, it is worth limiting rice. A good stimulator of lactation is carrots: fresh grated and in the form of carrot juice. But whole cow’s milk, contrary to popular belief, should be limited to 1-2 glasses per day. Fermented milk products are more beneficial for lactation.
For a sufficient amount of milk, the drinking regime should also be normalized: you should drink at least 2 liters of liquid per day, including soups, tea, and compote. About half of this should be clean drinking water. Drinking warm, weak tea half an hour before feeding stimulates milk production; adding ginger is useful.
Lactation is promoted by herbal teas from hawthorn, lemon balm, nettle, caraway, anise, oregano, sea buckthorn, and rose hips.
Dill tea helps with digestive disorders: 1 tablespoon of seeds should be diluted with a glass of boiling water and left for 1-2 hours, take half a glass 2 times a day. A drink made with cumin and anise is prepared in the same way. You can add honey to herbal infusions, but you should monitor the development of allergic reactions in mother and child.
The following should be excluded from the diet:
- flour, sweets, chocolate, preservatives;
- smoked, spicy, dried;
- products without sufficient heat treatment (half-raw meat and fish);
- alcohol;
- carbonated drinks;
- strong tea, coffee, chocolate;
- basil, sage, horsetail, lingonberry;
- Parsley and mint should not be consumed.
To normalize lactation, drugs are prescribed that stimulate milk production; as a rule, they are of plant origin, but they have their limitations for use and are prescribed after consultation with a doctor. In case of primary hypogalactia, when the lack of milk is caused by underdevelopment of the mammary glands and endocrine disorders, the mother is prescribed hormones - oxytocin or prolactin. Herbal preparations are indicated for secondary milk deficiency.
| A drug | Mechanism of action | Dosage regimen | Contraindications |
| Apilak | Based on bee royal jelly. It has a tonic property, enhances metabolism, and improves immunity. The preparation contains many vitamins and minerals, amino acids and biologically active components | 1 tablet under the tongue until dissolved 15-20 minutes before meals 3 times a day, milk flow an hour and a half after taking, do not take in the evening due to the tonic effect. Course – 10-14 days. |
|
| Mlekoin | Homeopathic medicine based on extracts: chaste vitex, stinging nettle, meadow lumbago | 5 granules in the morning and evening under the tongue 30 minutes before meals, throughout the entire lactation period | Hypersensitivity to the composition |
| Laktogon | Consists of oregano extract, dill, nettle, royal jelly, carrot juice, potassium iodide, vitamin C. Helps normalize metabolism and stimulate lactation | 1 tablet with meals 3-4 times a day, effectiveness increases if taken half an hour before feeding, 1 month | Bee jelly intolerance Diabetes |
| Leptaden | Consists of Leptadenia reticularis and Breynia extract, stimulates milk production | 2 tablets 2 times a day half an hour before meals. Swallow whole with plenty of water, 1 month | Individual intolerance |
| Glutamic acid | An amino acid that has a stimulating effect and also enhances lactation | 4 tablets of 250 mg 3 times a day 15-20 minutes after meals, combine with vitamin C 3 times a day of 250 mg, wash down with sweet tea, 1 month |
|
| Vitamin E | Affects the production of lactation hormones, the state of the reproductive and nervous systems, and pronounced antioxidant properties | 0.1-0.2 g 3 times a day, 1-2 months | Increased sensitivity Severe cardiosclerosis |
Features of breastfeeding after cesarean
Breastfeeding after cesarean section has its own characteristics: the baby often does not contact the mother immediately, sucking reflexes are inhibited, and milk may not be produced in the first time after the operation. You should strive to put your baby to the breast within the first hours after surgery, as this strengthens the bond between mother and baby, and also promotes the production of prolactin in the mother and strengthens the sucking reflex in the baby.
If the baby does not take the breast immediately and the reflex is inhibited, then you should try to give the breast every time the baby squeaks to ensure early feeding: the baby should be attached to both mammary glands for 15 minutes.
The first feeding of the newborn occurs after the operation, if the mother is conscious. The doctor or midwife places the baby on the breast and helps the mother to properly grasp the breast and place the nipple in the baby's mouth. You need to feed from both glands for at least 5-10 minutes. At this time, the baby’s nervous system is activated, and lactation is also stimulated.
The first portion of milk in the form of colostrum is 10-50 ml, which is quite enough for a newborn. There is no need to supplement the baby with formula during the first feeding, even if there is a deficiency of body weight. In the future, the midwife or doctor should explain to the mother how to properly feed the newborn, observing lactation techniques.
In Russian maternity hospitals, after surgery, mother and child are often separated, which makes feeding difficult. This should be taken care of in advance by discussing the details with your doctor. It is possible to stay in a shared ward, but the help of relatives will be required for feeding - the mother must protect herself from physical exertion after a cesarean section.
Difficulties also arise in spatial orientation after anesthesia. If the mother is not breastfeeding, then on the first day you can not pump, but start this process from the second day. There is no need to supplement the baby's feeding in the future if he receives some colostrum in the first days.
How to feed your baby
There are many recommendations on how to feed a baby; correct feeding technique is of great importance:
- A woman needs to take a comfortable position, undress to the waist and place the baby on her chest or on her arm if there is severe pain in the suture area.
- Then you should wait for a while, you can talk gently with the child so that both the woman and the baby get used to the new action. The baby's face should be directed towards the mother, the nose opposite the nipple, the body pressed against the mother's body.
- Support the chest with the index finger, the thumb is on top of the chest. You need to touch the baby's lips with the nipple, which will cause the mouth to open. The nipple should enter the baby's mouth, his lower lip should be below the nipple, the lips should be pulled back, the baby should take the areola more from below than from above, lips and gums are pressed firmly against the nipple.
- The next time you feed, you should change breasts. Feed until the breast is empty and the baby is full, which he will let you know.
The baby should be fed on demand, not on a schedule. To understand when to stop feeding, you need to pay attention to the baby’s behavior: he begins to suck weaker, turns his head and tries to “free” his mouth from the nipple. You can help the baby with your hand by carefully removing the nipple from the mouth. After feeding, the baby often falls asleep. Mom should wipe her breasts and massage them if necessary.
The mother must understand when the baby is suckling correctly: the lower lip is turned outward, the contraction of the muscles from the mouth to the ears is clearly visible. It is wrong if only the muscles in the cheek area contract. When the baby lets go of the breast, he should be offered a second one, since both need to be fed. The frequency of breastfeeding may vary and becomes more constant only after a month.
At night you also need to feed the baby on demand, this continues to stimulate lactation.
Low milk supply after caesarean section
There is no need to be upset because there is little milk in the breast. Usually, in the first 5-9 days, colostrum is released in small quantities - a very nutritious yellowish liquid. It is small in volume, but quite nutritionally sufficient for a newborn.
In order for lactation not to fade at the very beginning, a woman needs to periodically express colostrum, especially while she is in the intensive care unit and is not able to breastfeed the baby after a cesarean section.
Thus, the body receives a signal that milk is in demand and begins to produce it in large quantities.
In this case, you do not need to pay attention to how much colostrum is released from the breast during pumping; your task is to stimulate the breasts, and therefore ensure milk production in the future.
You don’t have to pump on the first day after surgery - rest while you have the opportunity. On the second day, start pumping at intervals of 2 hours, devoting 5 minutes to each breast.
You should be taught how to express your breasts in the maternity hospital. You should start with nipple stimulation; you don’t need to put too much pressure on the breast, and under no circumstances should you put too much pressure on the nipple. Using smooth movements, move your fingers from the base of the chest to the areola, evenly increasing the pressure. Focus on your feelings - it shouldn't hurt.
You can also use a breast pump: manual or electric. The latter option is preferable, as it imitates the baby's sucking rhythm.
After a caesarean section, it is recommended to drink a lot to replenish lost fluids. However, drinking too much can cause congestion in the breast when milk begins to actively flow. You should consult your doctor in advance on this issue.
If the baby is brought only for feeding, then breast fullness can turn into engorgement. In this situation, experts advise expressing milk 2 times a day until the breasts are completely empty (do not try to express every drop, milk is produced constantly).
When this method does not help, you can try to express as much as possible once a day (at 9 am or evening), and then every time, according to the baby’s feeding schedule, until you feel relief. Moreover, if the baby has sucked so much milk that you do not feel tension in the chest, there is no need to pump additionally.
Once the situation has stabilized, you can stop pumping completely and release your breasts enough to avoid discomfort.









