What to do if a nursing mother has urticaria?
Despite the development of medicine and the victory over many diseases, modern people still have many health problems. One of these problems is allergies and such a type as urticaria. The number of allergic reactions is steadily increasing. Medicines have been created that relieve symptoms, but it is not always possible to use them. For example, when a woman breastfeeds, she is responsible not only for herself, but also for the health of the baby, and medications from the mother’s body pass through the milk to the baby. In many cases, urticaria in a nursing mother can become a very serious problem, because you want to maintain natural feeding and not harm the baby. Unfortunately, in some situations it is not possible to combine these two needs, although in most cases the issue is resolved positively.
Causes of urticaria
In most cases, urticaria is allergic in nature.
Urticaria in a nursing woman can be chronic, that is, it was present before pregnancy. Then the patient must be constantly under the supervision of an allergist and follow the basic rules that will minimize or eliminate her contact with allergens, and be treated as prescribed. During pregnancy, a woman’s body changes a lot, and hormonal levels undergo special changes. This often leads to the appearance of allergies that were not there before, including hives. Usually, with the end of pregnancy, everything returns to its place, and allergy symptoms go away. However, in some cases, the allergy remains and is manifested by urticarial rashes (urticaria) during lactation.
Another scenario for the development of urticaria is also possible. The stress that the body experienced during childbirth led to changes in immune responses and the development of allergies, manifested by hives.
Science cannot yet accurately explain the global reasons for such changes. But it is possible to identify factors leading to manifestations:
- Temperature (cold or hot),
- Contact with fabrics or metals,
- Food,
- Animal waste products,
- Plant pollen.
Animals and plants rarely provoke an attack of urticaria; more often they cause a reaction in the form of rhinitis.
Rash on a newborn's body
All parents want to see their children beautiful, healthy and happy. If something goes wrong, for example, colic occurs, the temperature rises or a rash forms, dads and especially moms begin to panic. Young parents feel their own inadequacy and lose faith in their own strength. Although this is completely in vain.
The breakouts can be hormonal and usually look like regular red pimples. Pimples are localized on the cheeks, back and neck. There may be a small pustule in the center of the pimple.
A rash on a newborn’s body can form due to allergies. If a nursing mother does not watch what she eats and drinks, the baby may develop rashes on her face. Cow's milk is considered the strongest allergen, which is not something that can be poured into a bottle for a child, even a nursing mother should not drink it, especially in its pure form. You can also add it to tea, but you can’t just drink it. You should not eat red foods, because the red pigment provokes the formation of red pimples.
If the mother wraps the baby up too much, he may develop heat rash. Since the sweat glands are not yet fully formed, red bubbles appear in those places where the child sweats especially heavily.
A newborn has a rash on his body
A child is a modern creature, but in the first months of life it requires special care. If a newborn had a rash on his body, it could appear for a variety of reasons: from hormonal changes to external irritants. The most common causes of rash include:
- Adaptation to an aggressive external environment.
- Hormonal changes and removal of maternal hormones transferred in the womb to the outside.
- Incorrectly selected cosmetic products.
- Allergic reaction to medications.
- A reaction to inappropriate baby food if the child is artificial.
- Foods eaten by a nursing mother and causing rejection in the child.
- Miliaria or hives.
- The baby’s congenital predisposition to dermatoses, dermatitis and allergies.
In most cases, a rash appears on a newborn’s body due to completely natural reasons that can be easily eliminated. The exception is a genetic predisposition transmitted by parents and requiring long-term drug treatment.
Treatment of urticaria in nursing mothers
- Avoiding contact with allergens
- Taking medications
- Phytotherapy,
- Normalization of intestinal microflora,
- Hypoallergenic diet,
- Lifestyle optimization.
In the treatment of urticaria during breastfeeding, the safety of the child comes to the fore.
Therefore, treatment begins with stopping contact with allergens. If this is successful and the symptoms go away, then all that remains is to follow the appropriate regimen. In order to find out the provoking factors, you need to carefully analyze when and after what reactions occur. If these are food products, then you need to remove them from your diet; if these are some types of fabrics, then you should not wear clothes made from them. Hives can be caused by cold or fever. In these cases, protective measures must be provided. For example, use only warm water, dress warmly, and when going out into the cold, use protective creams for exposed parts of the body. It can be difficult to protect yourself from high temperatures in the summer heat. Then limiting walks during the daytime and installing air conditioning in the house will help. If all these measures are effective, then new manifestations of urticaria can be avoided, and you can do without medications. In some cases, the rash caused by hives does not last very long, just a few minutes. If no consequences or dangerous symptoms (for example, swelling of the larynx) are observed, then you can do without medications.
Itching Remedies
The hives rash is often accompanied by itching. If the rash causes itching that is difficult to tolerate, then you can use various remedies:
- Bepanten,
- Table vinegar (a teaspoon of vinegar per tablespoon of water),
- An infusion of a mixture of herbs: chamomile, elderberry, chickweed,
- cucumber juice,
- Aloe juice.
If the rashes occupy a large part of the body, then warm baths will help. You need to add vinegar or oatmeal to the water and soak in it for 10-15 minutes.
Medicines for nursing mothers
If urticaria during feeding causes severe discomfort in a woman, then it may be necessary to take medications that reduce its manifestations.
If a woman has urticaria during breastfeeding, she should not use hormonal drugs, even for external use. If you cannot do without them, then breastfeeding will have to be stopped.
Phytotherapy
- Valerian infusion,
- Camomile tea,
- Antihistamine tea from infusions of burdock, echinacea, nettle, marshmallow.
Antihistamines
You can read various recommendations on the Internet about taking antihistamines while breastfeeding. However, full-scale studies have not been conducted to study their effect on infants. It is known that all of them penetrate into breast milk, and therefore into the baby’s body. At the same time, only Zyrtec is approved for use in children older than 6 months. All other drugs can be given to children after one, two, three years. Thus, taking antihistamines by a nursing mother is possible only if the risk of the consequences of urticaria is higher than the risk of the drug affecting the child. Most often, when taking antihistamines, breastfeeding is stopped; if this is not possible, then the allergist decides the issue according to the circumstances.
Homeopathic remedies
Homeopathic remedies help many people well. They, as a rule, have no contraindications for breastfeeding. However, these drugs must be prescribed by a doctor, taking into account many factors.
Nutrition for urticaria
If a product causes hives, it is simply excluded from the diet. If the allergen cannot be identified, then a hypoallergenic diet is prescribed, which reduces the burden on the body and helps it cope with symptoms.
With a hypoallergenic diet, the following are excluded from consumption:
Vegetables and fruits with a high content of vitamin C are useful. Enterosorbents (activated carbon, Smecta, Polysorb) and preparations containing beneficial microorganisms (Lactobacterin, Bifidumbacterin and others) also have a positive effect.
Cause of acne
But it turns out that everything is not so bad. And acne is often a temporary phenomenon, because its cause is the hormonal changes that occur in the body of women after childbirth. The fact is that during pregnancy the level of female sex hormones estrogen and progesterone increases. Only during pregnancy is a female hormone called human chorionic gonadotropin produced.
And after childbirth - hormones that regulate the production of breast milk, in particular prolactin. And all these hormones gradually return to normal approximately one to two months after a woman stops breastfeeding.
This is somewhat comforting. However, despite the fact that time flies by quickly while caring for a child, you always want to look in the mirror and like yourself. What can be done to improve the condition of the skin and speed up the process of returning it to its previous state? Moreover, when breastfeeding, the choice of cosmetic skin care products must be approached very carefully.
How to deal with hives after childbirth and what can trigger it
Pregnancy and childbirth and everything connected with them are one of the most difficult and exciting periods in a woman’s life. They bring great happiness, but physiologically it is difficult.
A large surge of hormones occurs and throws the already greatly weakened body out of balance after pregnancy. Problems begin to arise.
Against this background, both acute and chronic diseases can develop, as well as pathologies that existed before can worsen. One of the fairly common diseases is urticaria after childbirth.
Causes of rashes on the body after childbirth
Pregnancy and childbirth place a high burden on a woman’s body. The immune system, like everyone else, undergoes significant changes. Decreased immunity is one of the mechanisms created by nature to prevent the mother’s body from rejecting a genetically foreign fetus that is half foreign. In some cases, the program fails and after childbirth the body gives an inadequate immune response to substances entering it.
There is no single cause for the rash. These include hormonal changes, disruptions in the digestive tract, allergic reactions, insufficient skin care and adverse effects of the environmental environment.
In a word, the rash of the rash is discord. And in order to successfully cope with it, you still need to find out the reason for its appearance.
Why does urticaria occur during lactation?
There are many reasons for the development of the disease. At the same time, the immune system deteriorates, the body weakens, and hormonal levels change. In particular, hormone levels greatly influence the body's ability to resist allergens.
During pregnancy, the hormone progesterone increases, and it is this hormone that is responsible for the manifestation of allergies. In addition, cortisol production increases. On the contrary, it acts by reducing allergic activity.
The woman’s future condition depends on the balance between these two hormones. Even those who have not previously suffered from allergic reactions may experience symptoms for the first time.
Factors that can trigger the disease
These include:
- The use of a large number of medications for childbirth.
- Consumption of foods that cause allergic reactions - allergens.
- Cosmetics and household chemicals that tend to cause dermatitis.
- Insect and parasite bites.
- Viruses, bacteria and fungi.
How to identify urticaria
If you suspect that you have a drip, you should consult a doctor to determine the cause. When contacting, the doctor will examine the patient and collect anamnesis in order to identify:
- How long ago did the rash appear?
- What provokes it and against what background it arose.
- What the patient consumes and whether she notices an improvement in her condition with the diet.
In addition, the doctor will examine the rash itself in order to rule out the presence of an infectious disease. Laboratory methods will also be prescribed to determine the nature of the pathology. These include:
- General blood analysis.
- General urine analysis.
- Blood chemistry.
When performing a general blood test, as a rule, an increased level of eosinophils is noted.
At the same time, ESR and leukocytes are normal. Tests for parasites and allergy tests are also prescribed.
Allergic rash - urticaria
Hives are itchy rashes and blisters that rise above the surface of the skin. A prerequisite for the development of the disease is a sharp jump in hormones during childbirth, and then their drop.
The impetus for the development of urticaria is the following factors:
- Medications
In particular, antibiotics and anti-inflammatory drugs. In some cases, hives begin after the end of treatment. For example, 14 days after starting medication.
- Food
These include highly allergenic foods: fish, nuts, chocolate, citrus fruits.
- Contact allergic reaction
When skin comes into contact with chemicals, most often household chemicals, an allergic reaction may occur.
- Insect bites
The rash after bites of insects such as hornets, bees, and wasps can persist for several days.
- Physical impact
An allergic reaction to cold, exposure to sunlight, vibration and water is often observed in people prone to various types of allergies.
- Stress
Nervous urticaria is also distinguished. After suffering stress during childbirth, a rash on the body may be a manifestation of urticaria.
Treatment of the disease
Only a doctor should diagnose the disease and prescribe treatment. Moreover, treatment is best carried out under his supervision. In addition, it is necessary to say that the child is fed breast milk, since the nature of the prescribed treatment will greatly depend on this.
What is urticaria, watch in this video:
For the same reason, it is very important that the treatment is comprehensive and as short as possible. The ideal option is to do without medications.
The most dangerous products in this regard are:
- Nuts.
- Milk.
- Eggs.
- The fruit is red.
- Some types of meat and fish are high in fat.
- Seafood.
- Butter.
- Citrus and exotic fruits.
In addition to diet, it is necessary to reduce contact with animals and plants. It is also important to use hypoallergenic cosmetics, natural clothes, use special powders when washing and not use fabric softener.
There are special cooling ointments and gels, some of which may be approved for use during lactation.
How to relieve itching
One of the most unpleasant manifestations of urticaria is severe itching. It is quite disturbing, and many people cannot tolerate it. Yes, and this can cause irritation, which is undesirable for a nursing mother when it’s already hard for her.
Therefore, it is necessary to try to remove it in all possible ways, namely:
- To do this, you can take baths from a decoction of chamomile and string.
- Use Bepanten ointment.
- Make lotions from aloe and cucumber juice.
- For small amounts of external rashes, you can use creams and ointments with a moisturizing effect.
- When the affected area is larger, non-steroidal anti-inflammatory drugs are prescribed.
- If they don’t help, then they use hormones, although this is highly undesirable in such circumstances.
As a rule, the doctor’s prescription does not include steroid drugs, which are contraindicated, but among antihistamines, he may prescribe:
They are used only as a last resort, but are not believed to pose a threat to the baby’s health. Treatment of urticaria in this case with homeopathic remedies is allowed. They do not pass into milk and do not affect the baby.
The principle of homeopathy is that like cures like. That is why very small doses of the allergen are used as a treatment for urticaria.
For homeopathy to really help, it requires an individual approach.
General medications will only affect external manifestations. And as you know, allergies are not limited to them. Therefore, it is necessary to find a good specialist to prescribe treatment.
Folk remedies against urticaria
However, their effectiveness is limited to use in a simple form of the disease that does not cause serious symptoms.
Since the main cause of hives is food allergies, it is recommended to first cleanse the body of toxins. To do this, you can use the following tools:
- Drink plenty of water and use chamomile infusion.
- One sip of castor oil.
- Nettle tincture.
- Celery juice.
In order to prepare the tincture, take 1 tbsp. l. dried plant and pour half a liter of boiling water. Next, infuse and filter. After this tincture can be taken. Do this 4-5 times a day, half a glass.
It is worth considering that you should not get too carried away with taking traditional medicine, as they can change the taste and smell of milk.
Also, any herbs that are used in recipes are generally safe, but in some cases they can cause individual intolerance. Therefore, before starting to take any folk medicine, it is necessary to do an allergy test.
This video will tell you how to treat hives:
The following are also recommended among traditional medicine:
- Take a bath with the addition of a decoction of nettle and elderberry, the leaves of which are taken in equal proportions.
- Prepare an ointment that relieves itching. To do this, chop the garlic and pour boiling water over it. Then simmer over the fire until the volume decreases by 2 times. Then add heated vegetable oil and a small amount of wax to make the ointment thick. After cooling it can be applied.
- You can also prepare a mint tincture and use it as a sedative. To do this, pour a few tablespoons of mint into half a liter of boiling water, cover with a lid and let it brew for an hour. Mint tincture is taken 50 milliliters 3 times a day.
Therefore, it is imperative to consult a doctor for help, especially if symptoms of serious disorders appear, such as Quincke's edema. In addition, there is no need to worry too much about the child’s health, since the disease is non-infectious, which means it is not contagious.
Why does hives occur after childbirth? Causes and treatment of urticaria during breastfeeding
Urticaria is an allergic disease that manifests itself in the form of a rash, which over time turns into swelling. It can occur anywhere in the human body.
We cannot treat this disease with the negligence we are accustomed to. After all, we see only the external manifestations of this disease, but the same thing happens inside our body. If urticaria is left untreated, blood pressure may rise, difficulty breathing may occur, and in general, everything can end in death.
But when a woman develops hives after childbirth and during breastfeeding, the problem arises of how to treat it without harming the baby. Since not all young mothers want to transfer their child to artificial nutrition.
Immunological rash
This type of rash is an allergic rash. Food allergies occur on the cheeks, less often on the body. A child can get an allergen through food while being both bottle-fed and breastfed. The latter means that the nursing woman consumed one of the types of allergens, to which the child’s body reacted. With artificial feeding, this indicates an incorrect selection of the formula and intolerance to some of its components. An allergic rash is most likely to occur when starting complementary feeding. To avoid serious consequences and know exactly which product causes an allergy, it is worth keeping a food diary. In it, the mother notes the introduction of new products and monitors the child’s reaction.

An allergy can manifest itself as a rash all over the body. Small red rashes appear in places where the child's skin comes into contact with allergens: pet hair, dust, and cosmetics. To avoid such a reaction, it is necessary to wash children's clothes only with baby soap and powder, and for the child use only special children's cosmetics that undergo strict quality control. But even this cannot protect against the occurrence of allergies.
IMPORTANT TO KNOW: How much does breast augmentation cost, and what methods of bust enlargement exist?
Dr. Komarovsky tells how to find the cause of allergies in the video below.
Causes
The first days after giving birth, a woman not only has to get used to a new way of life due to the fact that a new family member has been born, but also get used to her body again.
With the birth of a child, the mother's entire body is reborn. During labor, a hormonal surge occurs, leading to changes in the woman’s body. And if you have never had any allergic reaction, now it is quite possible.
Urticaria occurs as a result of:
- allergic reaction to food;
- contact with materials that cause allergies (clothing, jewelry, cosmetics, household chemicals);
- due to sudden climate change ;
- reaction to the sun;
- against the background of stress or hormonal imbalance, which is very important after childbirth, since the body is very weakened and the immune system fails;
- due to a malfunction of the stomach , liver or kidneys, a chronic form of urticaria may occur.
Hormonal rash

During the first days of a child's life, a rash may appear on the face and head, as well as throughout the upper half of the body. It looks like small pimples with a white tip. Such rashes are called neonatal pustulosis. They are absolutely harmless and go away on their own in the third month of the baby’s life. The reason for their appearance is hormonal changes in the baby’s body. The child’s body gets rid of the hormones it inherited from the mother through the surface of the skin. Thus, acne represents a child's natural adaptation to the outside world.
IMPORTANT TO KNOW: Early signs of pregnancy in the first week: changes indicating an interesting position
What is a hormonal rash in a baby, watch the video
Diagnostics: where to go, what tests will be taken?
There are three main types of urticaria:
- Physical - this includes mechanical urticaria, vibration, thermal contact urticaria, cold urticaria;
- Special – it includes aquagenic (from exposure to water), solar, physical stress urticaria, cholinergic urticaria, food urticaria, drug urticaria;
- Spontaneous - this includes autoimmune urticaria, urticaria (nodular vasculitis), complement-induced urticaria.
If you suspect that it is urticaria, it is best to contact an allergist to find out the exact cause of this disease. To do this, he must take allergy tests.
Most often, blood is taken for testing, but this method is too slow. It is better to carry out skin and provocative tests to get quick results.
So, urticaria in a nursing mother - treatment should begin immediately after an accurate diagnosis has been established.
What should you do first and what should you avoid?
You need to immediately give up foods that cause allergies - these are all fruits, juices, vitamins and any medications.
If you have been using creams, stop using them; perhaps one of the components causes such a reaction.
Try to have as little contact with detergents and cleaning products as possible.
Review your wardrobe and switch to clothes made from natural cotton fabrics.
In the future, when the doctor determines what type of urticaria your disease belongs to, treatment will be prescribed.
Itching Remedies
Hives cause very intense itching. If you can’t stand it, you can use:
- baths with chamomile decoction, string;
- cold lotions;
- Bepaten ointment;
- cucumber juice;
- aloe juice
What medications can I take?
During lactation, you should not use any hormonal or antihistamine drugs, but if you can’t do without them, you may be prescribed drugs such as:
Sulfur is a homeopathic medicine, but it can only be used under the strict supervision of a specialist.
Folk remedies
Traditional medicines are safe during breastfeeding. But they are effective only if the disease has not developed into an acute form.
Mostly, hives occur due to the consumption of any food products, so you need to cleanse the body of toxins.
- of castor oil will cleanse the body of toxins ;
- Chamomile tea and drinking plenty of fluids will help
- you can prepare a nettle tincture ;
1 tablespoon of dried flowers and nettle leaves are poured with ½ liter of boiled water, infused, filtered and taken half a glass 4-5 times a day.
- grate the celery root and apply the juice 1 teaspoon 2-3 times a day half an hour before meals.
If you have urticaria, you need a strict hypoallergenic diet.
The rash may appear on the leg, arm, face and other places.
Causes of rashes in an infant (photo and description)
During infancy, from 1 month to 1 year, the skin of infants is susceptible to many pathologies.
READ ALSO: Boil on the neck - causes of appearance and how to treat boils
This is caused by the following reasons:
- allergies;
- violation of hygiene rules;
- influence of maternal hormones;
- infections.
Hormonal rash – neonatal pustulosis
A small, red rash may appear in newborns in the first days and weeks after birth. This is the so-called hormonal rash.
The child’s hormonal system is rebuilt, begins to function independently and rejects the mother’s hormones.
Remnants of maternal hormones are released through the skin in the form of neonatal pustules. They look like papules with a white tip.

Usually located on the upper half of the body:
- head;
- forehead;
- cheeks;
- neck;
- back.
If proper skin care is not taken care of, a child may develop a fungal infection.
Separately, a rash is distinguished on the face and on the head (cephalic) in infants. They will be caused by the still imperfect functioning of the sebaceous glands or follicles and the simultaneous rapid proliferation of lipophilic yeast-like fungi such as Malassezia on the child’s face. Sometimes they are detected by light palpation.
The concern is that you may miss the signs and rashes caused by meningitis.
Signs of allergies
The appearance of a red rash on the cheeks of a baby primarily indicates the presence of an irritant.
- food products, drinks, mixtures;
- household items, clothing, toys;
- baby care products;
- environment, heat, cold, tobacco smoke.
After feeding, the mother will always notice the baby’s painfully pink cheeks and can guess what foods this happened after: those that she consumed herself or gave to the baby in complementary foods.

If a small red rash in a newborn does not disappear, merges, gets wet, crusts and peeling appear - you need to look for and identify the allergen.
Until the allergen is identified, the nurse herself must adjust her diet.
Avoid obviously allergenic foods:
- chocolate;
- citrus;
- honey;
- canned food;
- smoked meats
If the red rash and peeling on the face and body of the baby do not go away, you need to change the mixtures and carefully study their composition.
Additions to feedings should be done carefully, step by step. Start juices with drops, gradually increasing each day.
It is necessary to review the composition of creams, ointments, sprays, and powders that are used to treat the skin of babies.
Understand the toys, find out what material they are made of, who the manufacturer is.
Buy from natural fabrics:
- bed sheets;
- towels;
- blanket;
- diapers;
- baby vests;
- sliders;
- booties.
We need to find out if there are any smokers nearby. Maintain a constant indoor temperature.
Diaper dermatitis
Very often, children suffer from diaper dermatitis. It usually occurs on the body in places of contact with wet diapers, diapers, and diapers.
If you do nothing, the process progresses. Redness gives way to irritation, bright red diaper rash appears, and painful cracks form on it. Ulcers appear in their weeping gaps.
READ ALSO: Typhus - Medical Encyclopedia
The result depends only on proper care of the child. It is within the power of any mother to prevent such irritations.
If such a disaster has happened, it is necessary to more strictly control the hygienic care of the baby’s skin - wash it after each diaper change, bathe the child in string or chamomile, use baby creams and powders with zinc oxide.

Atopic dermatitis
Atopic dermatitis develops in children with a hereditary predisposition.
It will be provoked by food products entering the child’s body and the mother’s body during pregnancy and breastfeeding.
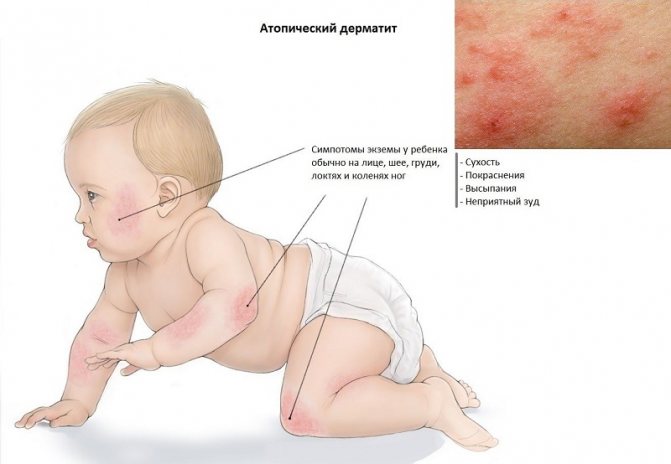
Scientists have found that the main allergen is whole milk protein. In second place are the proteins of soybeans, eggs, cereals, and fish.
The leading role in the development of dermatitis is given to the state of the digestive organs of the baby, the selection of food products of the mother during feeding and during pregnancy.
The child should not be overfed. Pasty children are more likely to suffer from atopic dermatitis.
The disease is dangerous because, starting with redness, peeling and itching of the cheeks and buttocks, the process expands and spreads, capturing the deeper parts of the skin on the body.
The resulting blisters become ulcers, the itching intensifies, greatly disturbing the baby.
Timely identification and elimination of the allergen will help to get rid of the disease faster.
Video from Dr. Komarovsky about atopic dermatitis:
Infectious rashes
Infectious rashes are caused by viruses, bacteria and fungi.
Fungal rashes are easily distinguished by the clear boundaries of clusters of small rashes. They quickly dry out, become covered with a white or yellowish coating, which is very flaky.
Among bacteria, a rash on a child’s body is most often caused by staphylococci and streptococci.
Infection with staphylococci manifests itself as pustular diseases.
Streptococcal infection is recognized by the appearance of a small red rash or blisters on the legs, arms, and face of a newborn. Blisters filled with exudate burst and the wounds dry out into crusts.
Viruses cause severe infectious diseases:
- measles;
- scarlet fever;
- chicken pox;
- rubella;
- Infectious mononucleosis.
The main signs of these diseases will be:
- heat;
- cough;
- a sore throat;
- nausea, vomiting;
- headache;
- abdominal pain;
- enlarged lymph nodes.
The rash will be a characteristic sign for each of them and distinguish them from each other.
Usually, rashes start from the scalp in the scalp, behind the ears, then appear on the face, cheeks, neck, and then go down to the body. They are found on the stomach, back, and buttocks. Then they cover the limbs up to the feet.
To make it easier to identify which infectious disease, here is a rash recognition table:
READ ALSO: Signs of the presence of parasites in the body of every person | Problem skin
| Disease | Type of rash | Color | Place and time of appearance |
| Infectious mononucleosis | Various in shape and size | Red | On the 5th – 6th day. On the face, less pronounced on the body. |
| Measles | Large spots, papules | Bright red | For 3 – 5 days. Appears behind the ears, along the hair, down to the feet. Step by step: face – torso – limbs. |
| Rubella | Small spots | Pale pink | Right from day 1. On the face, all over the body. |
| Scarlet fever | Small dots | Bright red on congested skin. Pale nasolabial triangle. | For 1 – 2 days. All over the body, worse in the folds. |
| Chicken pox | Spots, papules, blisters with liquid. Crusts. They develop gradually. Coexist at the same time. | Red | On the 2nd day. On the head, face, torso, mucous membranes. |
Treatment of urticaria during breastfeeding
Even rapid progress in modern medicine is not able to protect a person from the development of many diseases. Urticaria is one of the list of common diseases of an allergic nature. In pharmacies you can find a variety of medicines for internal and external use, but not all of them are safe for nursing women.

For many women, this condition can serve as a serious obstacle to natural feeding. With early diagnosis and proper treatment, young mothers not only get rid of the symptoms of urticaria, but also get the opportunity to continue breastfeeding.
The basis of this disease is an allergic reaction, which is caused by the irritating effect of various substances.
The following foods can provoke the development of an allergic reaction in a nursing woman:
- chicken eggs;
- sea fish;
- chicken raised under production conditions;
- nuts and sunflower seeds;
- biological food additives contained in products with a long shelf life;
- some vegetables and fruits (red and orange fruits and vegetables, as well as citrus fruits).

In addition, the following factors can cause the formation of urticaria:
- prolonged stay in conditions of low or high temperature;
- inhalation of plant pollen and household dust;
- contact with pets;
- taking certain medications (antibiotics);
- exposure to direct sunlight and vibration;
- entry into the body of pathogens of infectious diseases.
If an allergic reaction is triggered by inhalation of plant pollen, then urticaria is seasonal and makes itself felt during the flowering period of allergenic herbs and flowers.
You can recognize the occurrence of urticaria at home. At the same time, the nursing mother notices a specific rash (blisters) on the surface of the skin, which spread throughout the body and do not have clear boundaries. An allergic rash with urticaria is characterized by additional redness of the skin and itching.

When you press on such a blister, it turns white. From the point of view of classification, it is customary to distinguish between chronic and acute forms of the disease. The acute form of the disease is characterized by the appearance of an instant hypersensitivity reaction after contact with an irritant. In this case, the symptoms of urticaria disappear on their own after 1-1.5 hours.
The chronic form of the disease is characterized by cyclic exacerbation, which is provoked by repeated contact with the allergen and excessive emotional overload. The duration of exacerbation can be up to 8 weeks.
It is recommended to entrust the question of making a diagnosis to a medical specialist, since allergic urticaria has common manifestations with the following diseases:
- autoimmune pathologies;
- hepatitis types A and B;
- sepsis;
- helminthiases;
- diseases of the endocrine system.

During breastfeeding, care must be taken when taking medications. Treatment for urticaria does not differ from the treatment plan for other diseases of an allergic nature. First of all, a nursing mother needs to eliminate contact with a potential allergen.
The issue of taking antihistamines is resolved with the attending physician, since this group of drugs is not indicated for use during lactation. If a woman cannot avoid using antiallergic drugs, then breastfeeding is recommended to be interrupted for a short period of time.
For oral administration, you can use herbal preparations that have a sedative effect. Such means include:
- infusion of chamomile flowers;
- infusion of valerian roots and rhizomes;
- antiallergic herbal mixtures, which include nettle leaves, marshmallow root, echinacea flowers and burdock root.
Allergic urticaria is characterized by intense skin itching, which causes a lot of discomfort and interferes with full breastfeeding. The following drugs have antipruritic activity:
- Infusion of medicinal herbs (woodlice, elderberry, chamomile). The infusion is prepared at the rate of 2 tbsp. mixture of herbs per 300 ml of boiling water. The resulting mixture is infused for 1 hour. The strained and cooled infusion is wiped over the affected areas 4-5 times a day.
- Fresh cucumber and aloe juice. These components have a soothing, anti-inflammatory and antipruritic effect. For therapeutic purposes, it is recommended to wipe the affected areas of the skin with aloe or cucumber juice.
- Vinegar solution. To prepare the solution, mix table vinegar with drinking water in a 1:1 ratio. Use the resulting product to wipe the rash areas.
- Cream Bepanten. This product has a healing, anti-inflammatory, antipruritic and soothing effect on the skin. In addition, Bepanten protects damaged skin from pathogens. The chemical composition of the cream is absolutely safe for a newborn and a nursing mother.

Complex therapy for allergic urticaria includes not only drug treatment, but also compliance with dietary recommendations, as well as complete limitation of contact with irritants. Those foods that have allergic activity should be excluded from the diet of a nursing mother.
If the disease is mild and the woman does not need to take antihistamines, then she can safely continue breastfeeding without the risk of harming the baby.
Rash in a newborn: what to do?
Rash in a newborn is quite common. His skin is very delicate and sensitive to external irritants and internal factors. Should you do anything or quickly run to the doctor as soon as you see the crumbs of a rash on your skin? Let's find out!

Let's start with the fact that in the first three months of life, a rash in a newborn is a frequent and common phenomenon, it is caused by changes in hormonal levels. It is also called "neonatal acne." These appear to be small reddish pimples on the face, head, neck and back. This is a natural process, and there is no need to run to the doctor.
Never do the following if your newborn's rash is hormonal:
- do not dry with solutions of alcohol and potassium permanganate;
- do not use antibiotics and anti-allergy medications;
- Do not sprinkle talcum powder on the irritated area.
You can help your baby by bathing him in boiled water every day, ventilating the room and humidifying the air in it. And only when the rash occupies large areas of the body, you should consult a doctor. Typically, in such cases, a cream containing ketoconazole is prescribed.
At the age of three months to one and a half years, a rash in a newborn can be a symptom of “infant acne” - this is a sebaceous inflammation with a black dot in the center. You can’t do without a pediatrician here - he must prescribe treatment and monitor the results.
A rash on the body of a newborn can be a harmless prickly heat, a manifestation of an allergic reaction, or a symptom of dangerous infectious diseases, such as measles and scarlet fever.

Prickly heat
Clothing that is too warm and tight, and poor hygiene can lead to prickly heat - a rash of small blisters of fluid in the folds of the skin or in the groin, sometimes with itching. It is easy to overcome such a rash in a newborn - leave the baby without clothes more often, do not wrap him up, ventilate the room and bathe the baby regularly. A compress with soda solution will relieve itching.
Food allergies
The introduction of complementary foods or the consumption of allergenic foods by a nursing mother can cause a rash to appear on the cheeks of the newborn. It usually resembles blisters from a nettle sting. There is only one solution - try to limit the consumption of allergenic foods: cow's milk, citrus fruits, nuts, chocolate and brightly colored fruits, vegetables and berries.
Dermatitis
This is the skin's reaction to external irritants, such as washing powder, lint and pet hair. Choose hypoallergenic powder for washing children's clothes.

If the appearance of a rash on the child’s body is accompanied by deterioration in health, fever, diarrhea, fever or sore throat; If the rash grows throughout the body or fluid is released from the pimples, consult a doctor immediately! Most likely, this is one of the infectious diseases:
- chicken pox;
- roseola or baby fever;
- scarlet fever;
- measles.
During treatment, the child will need to be isolated from others and given medication, which only a doctor can prescribe!
Be attentive to your baby’s health condition and contact the clinic on time. Health to you and your child!
The danger of urticaria in a nursing mother, treatment
Urticaria is a fairly common disease from which no one is immune. Anyone can develop rashes and blisters, be it an adult, a child, or a woman while breastfeeding. In the latter situation, treatment of the disease requires a special approach. The disease can have several forms and types, which will determine the method of treatment and its duration. Urticaria in a nursing mother requires a special approach when designing therapy and selecting the necessary funds. You also need to follow your diet and doctor's recommendations.

Urticaria during breastfeeding requires special treatment
Why does the disease appear?
Basically, the appearance of hives is caused by an allergic reaction of the body. In a woman who is breastfeeding, it can be chronic and present until the baby is born. If this type of disease is present, it should be under constant supervision of the attending physician. It is also necessary to follow certain rules that will help avoid relapses. It is necessary to limit contact with allergens as much as possible and carry out periodic treatment. A pregnant woman's body undergoes significant changes. As a result, the balance of hormones changes, which is often the cause of hives. If a woman has not previously had any allergic reactions, they may appear during pregnancy. As practice shows, after the birth of a baby, the body returns to its original state and all symptoms of allergic reactions disappear. And there are also situations when everything remains unchanged and appropriate treatment is necessary. There are other possible causes of an allergic rash: stress experienced during childbirth. Due to emotional shock, a change in the state of the immune system occurs, which leads to allergies and the appearance of hives. The main factors provoking the development of the disease also include:
- temperature changes, hypothermia or overheating of the body;
- contact with allergens in the form of fabrics and metals;
- food allergies;
- medications that are not accepted due to individual intolerance;
- components of cosmetics, household chemicals;
- diseases of the thyroid gland and liver that have chronic forms;
- influence of stress, physical strain;
- the effects of animal waste products, insect bites;
- pollen of various plants.
There are many causes of urticaria, so it is necessary to identify and eliminate them, and then begin intensive treatment. Therapy should be based on the individual characteristics of the woman who is breastfeeding.

Household chemicals can cause hives
Causes of rash in newborns
Important! Most often, infants experience a minor physiological rash that does not require treatment and, as a rule, goes away on its own after a few days. But often rashes all over the body in children are provoked by infectious, viral diseases, and other exo- and endogenous factors.
A rash in a newborn baby can be caused by:
- hormonal disorders;
- disruptions in the functioning of the endocrine system;
- insect bites;
- improper care, violation of hygiene rules;
- infectious, bacterial, parasitic diseases;
- use of low-quality cosmetics and hygiene products;
- genetic disorders;
- disorders in the digestive tract;
- vascular dysfunction (vascular phenomenon in infants).
Often, rashes on the body of infants that occur in the first weeks of life are caused by hormonal changes in the body, increased activity of dermatophyte fungi, and yeast fungi.

Physiological rash in infants most often appears in the first weeks of life, which is explained by hormonal changes in the body
An allergic rash , which is quite often diagnosed in newborn babies on the arms, legs, face, is a kind of protective reaction of the body upon contact with any allergen.
Note. The problem of such rashes is most often caused by an allergic reaction to foods and medications that the mother takes during breastfeeding.
If the baby is bottle-fed, an allergic rash in the newborn can be caused by incorrectly selected ready-made formulas, namely certain proteins included in baby food.

An allergic rash in newborns during breastfeeding can occur due to the mother's poor diet
Important! In severe cases, with prolonged exposure to a strong allergen, for example, components of pharmacological drugs, Quincke's edema occurs. The rash does not go away for a long time, swelling forms on the child’s body, which can block the larynx, which will cause respiratory dysfunction.
Food allergies - a pink, red rash in a newborn - appears on the face, cheeks, chin, back, neck in the form of flaky small spots. With systematic exposure to allergens, the rashes begin to become weeping.

Diathesis, an allergic rash on the baby’s face, develops under the influence of proteins included in milk formulas
Drug rash in children is a side reaction of the body to taking pharmacological drugs, for example, antibiotics, hormones.
Note. Such rashes can also be provoked by multivitamin complexes.
Diathesis , manifested by a small red rash on the child’s cheeks, develops due to disturbances in the gastrointestinal tract. It can also be caused by instability in the functioning of the nervous system or represent a reaction to any external stimulus.
Hives , which manifests itself as a small red rash on various parts of the body of infants, are caused by various types of allergens - foods, medications, temperature factors.
Neonatal rash in newborns (newborn acne, neonatal cephalic pustulosis), which appears in the first two to three weeks after the birth of a child, occurs due to exposure to maternal hormones during embryogenesis.
Note. In boys, infant acne, which appears between the ages of three and 16 months, can be triggered by increased production of androgens, male hormones.
The cause of prickly heat lies in the imperfect thermoregulatory function of the skin of babies. Dermatological pathology can develop due to improperly selected clothing, failure to comply with hygiene rules, and as a result of overheating.
Contact rash (contact dermatitis) in infants develops in response to chemical allergens contained in washing powders that contain fragrances, when using conditioners, and rinse aids when washing clothes. The materials from which baby clothes are made can also cause small rashes all over the newborn's body.

Miliaria is one of the most common types of rashes on the body of newborn babies.
If peeling, small blisters, or a red rash are found on the butt of a newborn, this indicates the development of diaper dermatitis . The reason is prolonged contact of the epidermis with wet tissue, which provokes diaper rash.
Important! Physiological rashes in the first months in infants are most often caused by hormonal changes in the body. This rash does not require treatment and goes away on its own as soon as the baby is two to three months old.
The retention of sebaceous secretions provokes the appearance of sebaceous cysts in newborns, which are localized on the cheeks, chin, forehead, and less often on the arms and legs. Outwardly they resemble tiny papules of a light yellow, grayish color.
A small rash on a baby's ears is one of the symptoms of seborrheic dermatitis. Similar rashes in the form of greasy yellowish scales can appear on various parts of the body. The development of this pathology is facilitated by the excessive activity of opportunistic yeast fungi.
A rash in a newborn, localized in various parts of the body, can be caused by infection in the wounds if treatment with aseptic means is not carried out in a timely manner.

This is how contact dermatitis and diaper rash manifest in infants
How does the disease manifest?
Recognizing the disease is very simple. It can be either acute or chronic. In the first case, an allergic reaction occurs due to contact with an allergen or its penetration into the body. Symptoms may last from several hours to several days. In the chronic form, rashes appear constantly. They can be present for one and a half months. There are often cases when one allergen is excluded, and urticaria appears due to the action of another. The main symptoms of the disease include:
- the appearance of rashes and blisters on different parts of the body;
- feeling of severe itching;
- burning in the affected areas;
- sleep disturbance;
- high degree of irritability;
- nervous excitability.
You can recognize hives yourself. A breastfeeding mother may notice an unusual rash or blisters on the skin, which can be located in different areas of the skin. As a rule, rashes do not have specific boundaries. Symptoms also include redness of the skin in the affected areas and itching. If you press on such a blister, it turns white. At the first symptoms of urticaria, you should urgently consult a doctor, as this is fraught with consequences that will be very difficult to deal with.

Urticaria appears as an itchy rash
Rash due to infectious diseases
Childhood illnesses are often accompanied by rashes. The appearance of a rash on the head, then on the stomach, and then on the limbs may indicate chickenpox. The rash looks like small blisters with cloudy fluid inside. After they open, an itchy crust forms.
With scarlet fever, the rash is a rich red color, localized on the neck and upper body. They leave behind flaky spots.
With measles, the rash appears on the face and then spreads throughout the body. The spots are bright red and seem to protrude above the skin.
IMPORTANT TO KNOW: What types of facial peels are there: options and tips for choosing
If small red spots are added to the signs of the inflammatory process, spreading from the face throughout the body, then rubella infection is likely.
In any of the above cases, you must immediately consult a doctor and, after diagnosing the disease, begin treatment.

General treatments
Before starting treatment, it is necessary to undergo a thorough examination. There are many causes of hives. It may be a manifestation of some disorder in the body, and not just the result of an allergy. Treatment of urticaria in a nursing mother must follow certain rules. The therapy should not contain drugs that could harm the body or affect the composition of milk. There is now a large selection of allergy medications available, but not all of them are approved for breastfeeding women. It is very important to choose the right therapy that will help eliminate the symptoms of the disease, its cause and will not harm the baby. Therapy consists of the following mandatory actions:
- ensuring conditions under which there will be no contact with the allergen;
- taking special safe means;
- carrying out herbal medicine;
- normalization of intestinal function and ensuring good microflora;
- following a hypoallergenic diet;
- lifestyle adjustments.
When treating urticaria during lactation, the safety of therapy for the child is primarily taken into account. Treatment should begin only after the allergen has been eliminated. If it is possible to identify in time the cause of the problem and eliminate it, as well as the symptoms, the mother can only follow the established regime. Particular attention should also be paid to diet. It is necessary to exclude strawberries, various types of citrus fruits, chocolate, seafood, eggs, canned food, and all types of nuts from the diet. It is necessary to include foods containing vitamin C in the diet. In order to determine the negative impact factor that caused urticaria, it is necessary to carefully analyze in what period of time it appeared and under what conditions.
If these are food products, you need to remove from the diet those that can cause allergies. If it's about fabrics, then you should avoid wearing clothes made from them. Urticaria often appears when there is a change in temperature.
In these cases, it is necessary to provide appropriate conditions: wear warm clothes, use protective creams and warm water, limit exposure to the sun, install air conditioning in the room. If the creation of such conditions helps eliminate the disease and no new foci of inflammation are observed, you can do without the use of drugs.
People with urticaria should not eat chocolate
What medications should you take if you are sick?
If compliance with all precautions and elimination of factors has no effect on improvement, it is necessary to begin active treatment using appropriate means. Depending on the complexity of the disease and its form, the rash may be present for a long time or, conversely, for just a few minutes. If it goes away immediately and no additional symptoms are observed, you can do without medications. One of the obvious signs of urticaria is itching, which can be unbearable, which affects the psyche and causes excessive irritation. To get rid of it, you can use tools such as:
- cucumber juice;
- vinegar diluted with water;
- various herbal infusions;
- aloe juice;
- ointment Bepanten, as well as others.
If there is a lot of rash, you can take warm baths with vinegar or oatmeal. Not all medications are suitable for a breastfeeding woman, so it is very important that they are simple and safe, but effective. If discomfort during the disease reaches a critical level, it is necessary to use complex therapy. If conventional remedies do not help, you will need to take hormonal medications. In this case, breastfeeding will need to be stopped. Herbal medicine is aimed at calming the nervous system. It most often contains infusions of valerian, chamomile, and teas that have an antihistamine effect.

Bepanten ointment will relieve itching and irritation
Enterosorbents and drugs containing beneficial microorganisms also have a positive effect on the treatment of the disease. There is a certain list of remedies that can be used as a last resort if the health of a nursing mother is in danger. Their list includes:
The use of such drugs should be under the close supervision of a physician. Most often, they are used for Quincke's edema, at the time of identifying an allergic factor, as well as in cases where the cause of urticaria has not been found. You can also use topical agents, the list of which includes:
The duration of use of the drugs and their dosage are determined by the doctor. Very often, when treating urticaria during lactation, a regimen is used that involves taking antihistamines once a day, and then reducing the number of doses to once a week for prevention.
And also when treating rashes, preference may be given to homeopathic remedies, among which Sulfur is especially popular. Such drugs are not aimed at eliminating the problem, but at strengthening the body and accelerating the healing process.
During lactation, the use of gluconate and calcium chloride, which is administered intravenously, is often prescribed.
Urticaria in a mother can be treated while breastfeeding, so don’t panic right away. It is very important not to bring the disease to an advanced stage, when strong drugs are required, which will cause the cessation of the lactation process. If all recommendations are followed, the mother can continue to breastfeed her baby and completely get rid of the symptoms and causes of the disease. Don't neglect your health and your baby's future!