There is no worse situation in the home than when a child in the family is sick. Everyone is fussing, worrying, trying to create the most comfortable environment for him. But the baby is capricious and refuses even his favorite dishes, fruits and desserts. Consequently, he loses weight, which worries his mother even more, who tries to force-feed him, guided by the principle “the more food, the more strength for recovery.” But force-feeding cannot bring benefit not only to sick, but also to healthy children. Therefore, a nursing parent should refrain from such attempts, so as not to cause additional problems with the gastrointestinal tract, liver, kidneys and deterioration of the child’s health. How should you feed a child during illness, what rules should you follow when choosing a diet?
Proper storage
Breast milk can be stored at room temperature for several hours. The product does not lose its properties and is suitable for eating for 4, maximum 6 hours.
Storing breast milk
Once each pump date and time stamp must be in the container. The child's name should be mentioned if milk is provided to the child care provider. After pumping the suction pump, it should be thoroughly cleaned. Once the milk is completely frozen, the lid must be tightened in the container. At least an inch or so should be left above the level of the milk to allow it to expand as it freezes. Milk that will be used later must be cooled or emptied immediately.
To preserve breast milk for a long period, it must be placed in the freezer. In a deep-freezing chamber, milk remains of high quality for 6 months. In the standard frozen compartment, milk can be stored for 3 months. If the freezer is combined with a refrigerator, the storage period should not exceed 2 weeks.
Milk can be stored in small 2 to 4 ounce containers for later use. In the refrigerator, milk should be stored at the back of the freezer, not on the door. Milk can be refrigerated for up to three days at temperatures below 40 degrees Fahrenheit.
Use and save milk for defrosting
Breast milk can be stored in the freezer for 3-4 months at temperatures less than 32 degrees Fahrenheit. Milk can be stored in the freezer for 6 months or longer at temperatures less than 0 degrees Fahrenheit. To strain milk, before using one of the most important aspects, it is necessary to remember, first of all, to use the earliest expressed milk first. Breast milk does not need to be heated. It can be served at room temperature or cold.
Thawed breast milk should not be re-frozen, just like any frozen food. Therefore, it is most convenient to freeze milk in small portions (60-120 ml), which you can take out of the refrigerator one by one and use at one feeding.
Summarize
What to feed a child with a fever? The diet should be light - pureed vegetables/fruits, jelly, yogurt, low-fat cottage cheese, liquid porridge with water. Prepare dishes by steaming or in the oven, with the exception of compotes and jelly. This especially applies during the recovery period - you should not give fried foods.
You should not wake up a sleeping baby to give him something to drink or offer him something to eat. Sleep during illness is a wonderful healer; in sleep, the body restores its energy reserves. Do not try to feed your baby well - the menu should be rich in vitamins, food portions should be small.
During the recovery period, offer fresh fruits and juices more often, and buy a vitamin and mineral complex. However, remember that natural vitamins are valuable to the body, not artificial ones. Taking into account these recommendations, you can make your baby feel better during illness and during the recovery period.
In a refrigerator
If the mother is away from home for more than six hours, it is better to keep the expressed milk in the refrigerator. At temperatures from zero to five degrees, the shelf life increases to two days without loss of beneficial properties. It is not recommended to place the container on the refrigerator door or close to the edge. It is advisable to place it on a shelf as close to the back wall as possible.
Before feeding your baby, milk should be poured into an Avent bottle and warmed to room temperature. The nutritional quality will not be affected by this. Since milk can be stored for up to two days, mom can prepare five to seven servings in advance. After the specified period, it is unsuitable for use.
Defrosting
When you take the milk out of the refrigerator, it may be separated into layers. Don’t be alarmed, the fatty part just sank to the bottom, and the liquid part remained on top. This is an acceptable and normal process. Thawing breast milk should not be abrupt. Due to temperature changes, not only the beneficial properties of the product will be lost, but its taste will change.
Frozen milk, however, needs to be thawed. It can be thawed by leaving the tight container sealed in warm running water. Breast milk should never be heated in a microwave oven. Microwaves can overheat milk or create hot spots that cause burns, and more importantly, harm some of the beneficial foods, antibodies, and cellular components of breast milk.
It is normal for pumped breast milk to vary in color and thickness. The stored milk is separated into layers. The cream is heated to the very top when the milk is heated. Before introducing the milk, you should be careful to mix the milk cream.
Remove the milk from the freezer, rinse the residue off the bottle with warm water and place it on the refrigerator door. It will take approximately 8 hours for the milk to melt. If you need to defrost milk quickly, place the bottle under running warm water. Shake the bottle constantly to ensure even defrosting.
Thawed milk is best used immediately. If there is any left, put it in the refrigerator, where it can be stored for a day.
The milkshake is not recommended as long as it may break or damage some of the cellular components of the milk. The temperature can be checked by dropping a few drops of milk on the inner skin over the wrist. It should be comfortably warm. Breast milk containing lozenges should be used within 24 hours. If milk is left at room temperature, it must be used within 1 hour. Thawed milk should not be frozen.
Any breast milk left in the bottle after feeding should be discarded. This is because bacteria in the baby's mouth can degrade the quality of the milk and make it unsafe. So a 4 to 6 ounce storage is beneficial and reduces waste.
Heating
You can heat the milk under warm running water. Gradually increase the water temperature from warm to hot. Rotate the bottle slowly to ensure even heating of the liquid.
A simple and good method of heating is a water bath. Fill a small saucepan halfway with water and place it on the fire. Heat the water, but do not bring it to a boil. Remove the pan from the stove and place the bottle or container of milk in it. When the pan is not on the fire, the glass bottle can be placed at the bottom of the container. To ensure that the milk heats evenly, shake it periodically. In this way you can heat up both already melted and frozen milk.
If stored milk has a bitter or strange odor, or if there is any doubt about its insurance coverage, it should not be used. To store breast milk, either by hand or with a pump, it should be placed in a separate container, which can be purchased at pharmacies or in bottles and bags that can be sterilized at home and placed in the refrigerator, freezer, or freezer.
Breast milk is the most complete nutrition for a baby, helps it grow and avoid diseases such as allergies and even frozen milk is healthier than any artificial milk and therefore should not be wasted. Find out more: Benefits of breast milk for baby.
It is best to heat milk in a special baby food warmer. The device will quickly and efficiently defrost and heat the product to the temperature of mother's milk, without the risk of overheating. The heaters can operate from the mains or from car cigarette lighters, so it will be convenient for you to feed your baby while traveling. The heated product may differ slightly in color and taste, but this is normal and you should not worry about it.
To take breast milk, a woman must. Wash your hands with soap and water, massage your breasts with your fingertips, make circular movements around the areola, and remove milk by hand or using a pump. In the case of manual, you should place the bottle under the breast and apply pressure to the breast, waiting for a drop of milk. If you are using a pump, simply place it on your breast and turn it on while you wait for your milk to come out. After collecting milk, it is important to put the date and time it was taken in the container so that the woman can know if the milk is good to give to her baby.
When a woman produces enough milk, she should store it because her milk is the best food for the baby. Thus, it is important to always take milk after the baby has finished breastfeeding and at least 1 month before the mother returns to work, as it is used for the body to gradually produce more milk than a breastfed baby .
Do not defrost or heat breast milk in a microwave oven. It will lose its beneficial properties, and in addition, the microwave will heat the milk unevenly, and you risk burning your baby.
A supply of breast milk will help solve the problem of feeding your baby in your absence. Defrost and reheat milk correctly. Follow our recommendations and be sure to check the temperature of the product before giving the bottle to your baby.
How long can milk be stored?
Breast milk can be stored in the freezer for 15 days or in the refrigerator for 12 hours, preferably on the first shelf and never in the refrigerator door. However, opening the refrigerator or freezer may lower the temperature of the freezer and may degrade the quality of the milk, so it is recommended to avoid opening the refrigerator or freezer frequently. Find out more at: Breastfeeding.
Milk storage container
The collected milk should be placed in its own container, which can be purchased from pharmacies, which is tightly closed, sealed and sterilized. Learn how to sterilize: How to sterilize a baby's bottle and pacifier. These containers must be filled, leaving 2 cm of fill at the closing edge, and milk from different feeds can be in the same container until the volume of the container is completed, but the date of first milk withdrawal must be recorded.
The life of modern women is filled with a huge number of events. Many active mothers do not want to drop out of life after childbirth and stay with the child all the time. They have to combine work, family, child care, and household chores. Fortunately, a huge number of useful household appliances allow them to do this. You can throw dirty diapers into the washing machine, food into the slow cooker, start the robot vacuum cleaner and that’s it. All household chores are done by themselves. However, childcare is not that simple. If a young mother leaves home, she must take care of what her little child will eat while staying with the grandmother or nanny.
How to defrost breast milk
To defrost breast milk, you must. Use milk that has been stored for a long time and should be used within 24 hours. Remove milk from the freezer several hours before using, defrost at room temperature or in the refrigerator. Place the bottle of milk that the child will drink in a pan of warm water and let it warm up in a water bath. If there is more milk in the storage container than the baby will drink, he should heat only that which will be consumed and keep the rest frozen, as milk should not be frozen again after thawing and playing with the remaining milk from a bottle or glass.
Of course, the easiest way is to feed your child an adapted formula. However, why do this if the mother has a lot of her own healthy and irreplaceable milk. Everyone knows that breast milk is involved in the development of strong immunity and protects against the development of various allergic reactions. And in general, if a woman is not yet going to stop breastfeeding, why give formula? You just need to know how to properly express, store and heat milk.
How to transport frozen milk
Frozen milk should not be heated on the stove or in the microwave because the heat is not uniform and can cause burns in the baby's mouth and destroy the milk proteins. If a woman has been taking milk and must be transported from work to home, for example, or while traveling, she should use a thermal bag and refresh the ice every 24 hours.
To properly store breast milk, it is important to know that you must store the milk in a specific container for that purpose and be very careful when collecting, storing and using the milk to avoid contamination. The following images show glass breast milk containers and pouches that can be found in specialty maternity and baby stores and online.
what to feed a baby at a high temperature
The health of the child is the priority of every mother. Therefore, young parents will be interested in this page, which is entirely devoted to the question “how to reduce a child’s temperature.” We will talk about the reasons for the increase in the baby’s body temperature and methods for lowering it. Have a pleasant and useful reading!
Let's start with how to correctly measure a baby's temperature. It is measured in the baby's armpit using a mercury or electronic thermometer for three to four minutes. Or it is measured with the same thermometers in the rectum, that is, rectally. The second method gives the most accurate indicators of the baby’s body temperature.
Normal body temperature in children is considered to be 36-37 degrees. Deviations within these limits depend on many factors: age, time of day, child’s behavior, food intake, ambient temperature, and so on. A healthy child can have a body temperature above thirty-seven degrees. This happens in infants in the first months of life, when the baby, wrapped in diapers and a blanket, is in a hot, poorly ventilated room, or in children who have been in the sun for a long time. In older children, an increase in temperature is possible after very active games. In such cases, it is enough to unwrap or lightly dress the child, let him calm down, and after twenty-six to thirty minutes the child’s body temperature will become normal.
The fact is that a temperature reaction is a normal response of a patient to an infection or some other aggression. It is known that some microbes are even killed by high temperatures. However, a fever (this is the same as a rise in body temperature) is considered dangerous if its degrees in degrees exceed those indicated for a certain age and it lasts more than two hours.
Parents are required to seek medical help immediately at any time of the day if an increase in body temperature is combined with:
1) with the fact that the skin began to turn pale,
2) convulsions,
3) blackout or loss of consciousness,
4) lethargy or indifference to others.
A few words about attacks of so-called unexplained fever and a prolonged slight increase in temperature.
A condition when, against the background of absolute well-being, the baby’s temperature rises to 38-39 degrees and, persisting for two to four days, also suddenly and without treatment drops to normal numbers, is called unexplained fever. A prolonged low increase in body temperature is when a temperature of 37.1-37.5 degrees lasts for weeks, without outwardly affecting the general condition of the child. Both conditions should not be ignored by parents and require a visit to a doctor for a thorough examination so as not to miss serious diseases.
It is imperative to mention an increase in temperature as a symptom of teething in a baby. Indeed, at the site of tooth eruption, biologically active substances are released and local inflammation develops. However, the temperature rises only for a day or two, and there are no further symptoms. In any case, only a doctor can determine this by examining the child and excluding all other possible causes of fever.
If the readings are above 38 degrees in children in the first two years of life or above 38 and a half degrees in children over three years of age, but in the absence of these symptoms, you can use some home remedies to reduce fever.
The lower the room temperature, the higher the heat transfer. Be sure to ventilate the room in which the child is located, taking him out of the room at the time of ventilation. The ideal indoor temperature is plus twenty degrees Celsius. In addition, the air must be humidified. The optimal room humidity is about 60%. If you don’t have a humidifier, wipe the floor more often and hang wet towels in the room. If there is a heating season, we recommend that you place wet towels or diapers on heating radiators. This way the room is humidified faster.
In a well-ventilated room, but without drafts, undress the child and cover him only with a light sheet or diaper, perhaps keeping it slightly damp. If you have a fan at home, direct the air flow towards the patient. Dry your child with a towel moistened with lukewarm water. If the child is very small, wipe him in the places where large blood vessels pass and the body. Rubbing for a few minutes can reduce the temperature by half a degree, and sometimes even a degree. Do not wipe your child with vodka or vinegar - you can cause skin burns and also cause poisoning of the body. Apply a cool compress to your forehead, changing the cloth periodically as it warms up.
Among antipyretics in children, drugs based on ibuprofen or paracetamol can be used. They are available in syrup and candles. Their effect occurs within twenty-five to forty minutes. Do not exceed the single and daily dosage indicated in the annotation. Under no circumstances use drugs based on analgin, which is part of the lytic mixture, or aspirin. You should not alternate taking drugs based on ibuprofen and paracetamol (choose one), as this can lead to an overdose and increases the likelihood of side effects.
If a child is vomiting, then giving syrup is pointless. Be sure to give your child plenty of cool liquids to drink - water, tea, fruit juice, compote. Drinking plenty of fluids also helps reduce fever. Ensure that your child urinates frequently and that the urine itself is light-colored. But you shouldn’t feed a child “through I don’t want to.” It’s okay if the child doesn’t eat anything during a period of high fever. You can do an enema. This is also a method of reducing temperature.
If a child feels well against the background of elevated body temperature, is active, plays, does not complain of pain, and the thermometer has not risen more than 38 - 38.5 degrees, pediatricians do not recommend giving the baby antipyretics. Fever is usually a response of the immune system to an infection that has appeared in the body. That is, when there is a fever, the baby’s body more actively fights harmful microorganisms. Parents should not panic or worry if the baby tolerates the increase in temperature normally, continuing his normal lifestyle with games and physical activity.
You can repeat taking the medications only after 4-5 hours. If there is no effect from taking medications or physical methods to reduce your temperature, do not tempt fate and seek medical help.
Many parents incorrectly think that if they do not give an antipyretic drug, the child’s body temperature will continue to rise. This is wrong. Most parents are convinced that high temperatures are dangerous for the baby’s brain. Pediatricians say that temperatures above 42 degrees are dangerous for the brain, which is never reached during ordinary infections. Such a temperature can only occur against the background of overheating of the baby.
Expressing breast milk
Nursing mothers resort to pumping for various reasons:
- Lumps form on the chest caused by blockage of the mammary glands;
- a nursing mother has urgent matters outside the home and cannot feed the baby on schedule;
- excess milk that remains in the breast after feeding;
- maternal illness and hospitalization;
- to stimulate the breast if there is very little milk.
Before expressing, a woman is recommended to drink hot tea with milk or take a warm shower. It is also necessary to massage the breasts to stimulate the process. Several pumping options are possible:
- Using a breast pump. The device must be sterilized and dried before use. Breast pumps come in electric and manual versions. The choice is determined by financial capabilities and personal preferences. It is also recommended to pay attention to the ease of disassembly, the strength of the vacuum created, the list of components, the popularity of the brand, and ease of maintenance.
- Manual method. A simple method used by most breastfeeding mothers. First you need to thoroughly wash your hands with soap and prepare a sterilized container with a wide neck. Next, you will need to press your hand to your chest and, after massaging it, begin to stimulate the milk ducts with two fingers. If the amount of expressed milk is insufficient, the procedure must be repeated exactly with the second breast.
Having mastered the intricacies of the process, young mothers quickly learn to select the optimal rate of pumping so that milk can be stored in reserve and the baby will have enough during breastfeeding.
How to maintain lactation during treatment
If the disease allows you to maintain lactation, you must continue to feed as usual, as before the disease. In a situation where the doctor has prescribed a temporary interruption of lactation for the period of therapy, you should pump regularly. This way the milk will not go to waste, since the need for it will not decrease. After recovery, you can continue to feed successfully.
Not so long ago, there was a time when, if a mother was ill, they were advised to boil expressed milk and, after heat treatment, give it to the baby through a bottle. Modern pediatricians categorically insist not to do this, since after boiling all the beneficial microelements from milk disappear, and it has no biological value.
If the mother is taking medications that are not compatible with feeding, or the infection is severely bacterial, the expressed milk should be discarded. During this period, the baby must be switched to artificial nutrition and fed with infant formula. After recovery and consultation with your doctor about the time period for complete removal of medications from the body, breastfeeding can be continued.

Pumping to maintain lactation
An increase in temperature in a nursing mother is not always a reason to interrupt or even stop breastfeeding. Sometimes a child can and should continue to be fed at a high temperature. This is what allows him to more easily endure the infection and develop protective immunity. The diagnosis of a disease of which hyperthermia is a symptom should be made by a qualified physician.
What temperature is considered normal for a nursing mother?
A woman who monitors her body temperature during pregnancy may notice that after childbirth, it changes: the thermometer begins to show 1–1.5°C higher. This is physiological and is associated with the arrival of milk, so mommy should not be scared and take action. Jumps in body temperature occur even during feeding: usually before feeding, the readings on the thermometer are higher than after feeding or pumping.
Breast milk is a substance with pyrogenic (temperature-raising) properties. The more it accumulates in the thoracic ducts, the higher the temperature will be. And if the thoracic ducts are damaged or infected, the temperature rises to 39°C.
To find out the exact temperature of a nursing woman, the measurement should be taken no earlier than half an hour after feeding. The norm is 37–37.1 degrees. During feeding, the normal value increases to 37.4°C.
In the first month after childbirth, women experience breast pain, and sometimes the pain is accompanied by low-grade fever. If there are no seals, do not worry - during this period the chest canals expand, which causes pain.
Why continue breastfeeding
The baby is weaned from the breast in the most extreme cases, when medications are incompatible with lactation, or if there is a risk of transferring the infection to breast milk. There are often situations when the benefits of breastfeeding for a child outweigh the possible risks, so doctors recommend continuing and maintaining lactation during treatment and even hospitalization. It is necessary to continue feeding or express milk regularly to be able to bottle feed your baby.
Important information! If treatment is carried out with antibiotics, you can stop feeding for a while and switch the child to formula, but it is important to express milk up to 6 times a day (according to the number of feedings). This will avoid stagnation of milk and resume feeding after healing.
What does elevated temperature indicate during lactation?
Elevated temperature during feeding may have the following characteristics:
- Physiological.
- Pathological.
The physiological process is associated with the production of milk by the mammary glands.
Doctors consider a temperature above 37.6°C to be pathological, which lasts for a long time and is accompanied by other symptoms of illness.
The most common sign of fever immediately after the birth of a baby is complications during childbirth:
- suture dehiscence after cesarean section or episiotomy;
- endometritis;
- postpartum thrombophlebitis;
- stagnation of milk (lactostasis) in the mammary glands.
The postpartum period is considered critical, because a woman goes through a difficult journey, which is fraught with a lot of complications. Open birth canals, ruptures, hormonal shock - this is a list of not all dangerous conditions. Any of them allows the infection to easily penetrate the mother’s body, so the temperature of a nursing woman is one of the important markers of her health status.
Childbirth often begins a series of various inflammations: endometritis, mastitis. This list also includes postpartum thrombophlebitis - inflammation of the venous wall, as a result of which blood clots form inside the vessel. This is a very serious postpartum complication, the marker of which is temperature and corresponding symptoms.
Fever often accompanies a cough, runny nose, and sore throat. Colds are the most common cause of high fever. This is followed by stagnation of milk in the breast (lactostasis). Lactostasis differs from mastitis in the absence of swelling and hyperemia of the mammary gland. Once the outflow is restored, fever and pain disappear without treatment.
The main symptom of mastitis is the presence of a painful lump in the breast and redness of the skin over it, which is accompanied by an increase in temperature to 38 °C. If you do a blood test, the ESR will be increased and the leukocytes will be increased. There is severe intoxication with malaise and headache. Without treatment, purulent mastitis develops.
When to stop breastfeeding
The issue of continuing guardianship or a temporary break should be decided after a doctor’s examination. It is necessary to evaluate and weigh the risks that are possible for the child if the mother is ill and takes medications.
When is breastfeeding allowed?
In case of the following diseases, accompanied by elevated temperature (increased within reasonable limits, up to 38 °), lactation can and should be maintained:
- With acute respiratory infections and acute respiratory viral infections, sometimes called “colds,” a nursing mother, in close contact with her child, in any case transmitted the virus to him. As the temperature rises, the female body begins to produce interferon to fight the virus. Antibodies also penetrate into milk, so the baby either will not get sick at all, or will easily tolerate the disease, developing protective immunity for the future;
- Lactostasis and mastitis in the early stage (not purulent) are not reasons for interrupting breastfeeding; on the contrary, successful treatment requires regular emptying of the breast; otherwise the chest will overflow and cause an even higher fever;
- A mild intestinal infection goes away after the gastrointestinal tract is completely cleansed of toxins. This happens within a day if you follow a diet. Feeding should be continued to develop antibodies in the milk to the infection.
When should lactation be stopped?
Most diseases do not pose a risk to the baby, and lactation can continue. However, there are a number of diseases in which feeding will need to be interrupted for a while. These include:
- pneumonia;
- purulent sore throat;
- purulent mastitis;
- cystitis;
- severe form of intestinal infection;
- dysentery.
Due to the serious condition of the mother with such diseases, milk production may decrease, but it still requires a sufficient amount of energy. Therefore, first of all, treatment is necessary. A significant increase in temperature is caused by bacterial infections that are treated with antibiotics. By themselves, they are rarely compatible with lactation and can cause allergies and dysbacteriosis. Diseases are also dangerous for the baby due to toxins that penetrate into the milk. For a newborn baby, this will have a detrimental effect on the condition.
How to collect and store breast milk
If a woman leaves home and leaves the baby for no more than 6 hours, she can express fresh milk in advance and leave it at room temperature. This milk does not lose its properties and is absolutely safe. If the mother is separated from the baby for a longer period of time, the milk should be placed in the refrigerator. This milk can be stored for no more than four days. Before giving milk to a baby, it needs to be warmed.
Before you take the milk, you must set the date and time to remove the milk, and then begin the extraction process. After extracting the milk, you should close the container and place it in a bowl of cold ice and pebbles for about 2 minutes and then store it in the refrigerator, freezer, or freezer. This treatment ensures that the milk cools quickly, preventing contamination.
The shelf life of breast milk depends on where it is stored. Ambient temperature - 40 minutes. . Some important recommendations are not to re-release breast milk that has been at room temperature for more than 30 minutes, as well as any remaining milk that may remain in the bottle. However, it is possible to reconstitute milk if the container has not yet been used and if it has been in the refrigerator for less than 48 hours.
It happens that a mother will have to undergo long-term treatment, surgery, or other reasons why she will not be able to feed her child for some time. Then she needs to stock up on a large amount of breast milk several weeks in advance. To do this, you need to buy special small containers at the pharmacy, approximately 100-150 ml. The size is not accidental - children under six months old eat exactly that much at one feeding, and since milk cannot be reheated, this container volume is very convenient. In addition, special containers are made of safe plastic that does not change the taste and smell of the product.
Remove the milk from the freezer or freezer a few hours before using it and let it defrost slowly, placing the container in a bowl of warm water to keep it at room temperature. To find out the temperature of the milk, you can put a few drops of milk on the back of your hand. Give the milk to the baby in a properly sterilized bottle and do not reuse the remaining milk from the bottle because it has already come into contact with the baby's mouth and may not be suitable for the baby. consumption. Frozen milk should not be heated on the stove or in the microwave because it can get hot, ideally it heats the milk in a water bath.
You can express milk by hand or using a breast pump. Women who go to work do this during their lunch break to free up their engorged breasts. Expressed milk should be placed in the freezer. There it can be stored for up to several months. This way you can make decent reserves, especially if a woman has a lot of milk. This allows you to feed the baby regardless of the mother's presence.
After maternity leave, they begin preparations for returning to work. Start looking for solutions to prevent your child from being harmed by your new routine. One of the problems is how to feed the baby during working hours. If possible, take your baby with you to work to breastfeed. One option when it is not possible to take your baby to work is to extract breast milk to feed him later. This milk withdrawal should be done two to three times a day and stored in a clean container.
This selected milk can be stored at room temperature for eight hours without porting and can be given to the baby in a clean cup. But be careful: you should not replace breast milk with other foods. When you are already at the stage where you should include foods with breast milk after 6 months, it is recommended that you consult a nutritionist or pediatrician to advise which foods are most appropriate for each stage of your baby's life. Also try to offer healthy foods made at home, avoiding industrial ones.
Temperature during breastfeeding
Each of us knows what exactly needs to be done at the first signs of a cold. But when chills appear and the temperature rises during breastfeeding, this inevitably raises fears of harming the baby. Young mothers are at a loss as to how to help their body as soon as possible and are looking for the cause of the elevated temperature. Elevated thermometer readings may indicate that a nursing mother has a cold, but there are other reasons, which a qualified specialist will help you determine. Temperature fluctuations can occur in the first weeks after birth, but let your doctor decide how dangerous they are. If a nursing mother has not visited public institutions with large crowds of people in the near future, then postpartum inflammatory diseases or exacerbation of chronic diseases should not be ruled out. Self-medication in such cases is dangerous, as it can worsen the problem. One of the reasons may be lactation mastitis, when inflammation in the mammary glands is observed against the background of general weakness of the body with an increase in temperature. This disease cannot be treated without taking antibiotics.
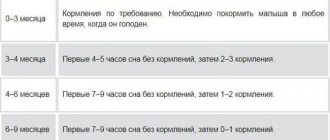
Feeding scheme and rules
Feeding with expressed milk from a bottle is carried out according to the same schedule as in the case of putting the baby to the breast. Pediatricians advise feeding newborns on demand. On average, babies need food every 2-3 hours.
It is important to follow the rules for bottle feeding your baby:
- the container into which the liquid is poured and the nipple must be clean;
- Milk should be offered to the baby fresh and of high quality. Do not give a product that has been stored in inappropriate conditions.
Experts recommend following the following bottle feeding algorithm:
- warm breast milk. The optimal liquid temperature is +34-36 degrees;
- take the baby in your arms and give him a reclining position;
- Offer your baby a bottle with a nipple. The baby should be fed at intervals of 2-3 seconds;
- hold the baby upright for about 3-5 minutes. This is necessary so that the air swallowed during feeding comes out and bloating does not occur.
Fever with vomiting
What to do if a child starts vomiting? What should the diet be like? In this situation, only drinking regimen is indicated. When vomiting, the body loses energy, so you should not give your baby food - he will still vomit again and lose additional energy. The same applies to infants: a nursing mother needs to follow a diet when the baby is sick and not eat fatty, indigestible foods.
Sometimes when vomiting, the best remedy is to drink warm boiled water. When the vomiting stops, offer juice or liquid jelly. Observe the body’s reaction and the baby’s desires - he will choose what is best for him to drink or eat in a given situation. You can’t drink in large quantities either - drinking should be fractional. Offer half a glass of compote or water.
How to warm up breast milk
Human breast milk should not be boiled. At the same time, it loses its vitamins and becomes useless. If milk is frozen, it should be defrosted gradually, without sudden temperature changes. Simply place the container of milk from the freezer into the refrigerator. Once it has completely melted, you can reheat it. You can do this in various ways.
Check guidelines for extracting and storing breast milk. Preparing a bottle for storing milk. Wash the glass bottle with the plastic cap, removing the label and paper from inside the cap. The ideal is to leave a few jars ready. These can also be bottle sterilizers, which are containers suitable for this function, in faster and more practical ways.
- Place the jar and lid in a saucepan, covering it with water.
- Cook them for 15 minutes, counting the time from the start of boiling.
- Drain onto a clean cloth until completely dry.
- Close the bottle without touching the inside of the cap.
How to store collected milk?
Hot water This is the easiest and most optimal way to warm up a bottle of milk. Just place it under running hot water and shake it periodically. The milk will become warm in a couple of minutes. It happens that you urgently need to heat up frozen milk, but there is no time for long thawing in the refrigerator. In this case, you need to place the container with milk under running cool water. And only after the milk has completely melted can it be heated with hot running water. This is done in order to preserve beneficial enzymes.
Water bath You can warm breast milk using a water bath. To do this, put a pan of water on the fire and wait until it boils. After this, place a smaller pan on top so that its bottom is above the steam. The pan should not boil too much, otherwise the milk will heat unevenly. This is the safest way to heat food, because there are no extremely high temperatures in a water bath.
Special heater There is a special device that runs on steam. It is multifunctional and very useful for a young mother. It can be used as a bottle sterilizer and also for heating cold milk. In the future, when the baby begins to eat complementary foods, this device can be used as a steamer for preparing lean food.
The bottle warmer heats milk very quickly and safely. The main thing is that it prevents overheating and gives a signal that the milk is ready when its temperature reaches normal.
Stir the milk thoroughly because it may not be fully heated. Whatever method you use to warm breast milk, be sure to check it before you give the bottle to your baby. Place a few drops of liquid on your wrist - the milk should feel warm and comfortable.
Is it possible to heat breast milk in the microwave?
There is a lot of controversy on this topic. When milk is heated in the microwave, it loses all its beneficial properties, vitamins, and enzymes. Such milk, of course, is not harmful, but absolutely useless. In addition, the microwave may heat the food unevenly, which can lead to overheating if it is not shaken well before feeding. Watch the time carefully. Do not microwave milk for more than a minute as it may curdle and cause problems with your baby's stool. Let heating in a microwave oven be possible for you only in the most acute situation - when the baby demands to eat here and now.
There are several tips that are useful to use when storing and heating milk.
- Do not store breast milk on the refrigerator door. The temperature there is higher, and the door is constantly opening, and hot air is blown over the milk. This worsens its properties. It is better to store breast milk in the back of the refrigerator.
- Thawed milk can be used for more than just eating on your own. You can use it to dilute porridge and add it to purees. This is not only useful - breast milk in food allows the baby to feel a familiar taste and begin to eat complementary foods with pleasure.
- Sometimes, after defrosting, milk loses its usual taste and color. This is normal, there is nothing wrong with it.
- If you notice that the milk has separated into layers, do not worry, this is also normal. This way, by the way, you can determine the fat content of your milk. The thicker the top layer, the fattier the milk.
- If you are afraid that you will give your baby milk that is too hot, measure the temperature of the liquid with a thermometer. The temperature should not be higher than 37 degrees.
- Milk should not be reheated or frozen.
Breast milk is both food and drink for a baby. When properly frozen, milk retains 95% of its beneficial properties. Proper heating of milk will help you not deprive your baby of valuable vitamins, even if you are not around.