Chest pain is one of the most unpleasant sensations that girls experience. Simply because many of them do not know where it comes from, and, as a result, think about something terrible. "While girls tend to associate chest pain with terminal illnesses, most often they have nothing to worry about," says Raquel Dardik, MD, of New York University.
If you are experiencing chest pain (especially if it is sudden, severe, or accompanied by lumps), it is best to see a doctor as soon as possible. If the painful sensations cannot be called acute, check the list below and act based on the information received. Here are five things at once that can cause discomfort in the chest, but do not require an urgent appointment with a mammologist.
Menstrual period
“Breast pain comes and goes with your cycle and is caused by the monthly hormonal shifts you experience,” explains Raquel Dardik. Some women are more sensitive to these changes than others (so they experience this pain regularly), while others experience this experience several times over the course of time (or never). The classic case is pain 10 days before menstruation, but this period may vary from person to person. In addition, you may feel swelling in your breasts, which usually goes away immediately with your menstrual period. Remember that any major hormonal changes, including pregnancy and menopause, can cause breast pain. Although the pain in these cases will not be cyclical, it may still come and go.
Chest examination after injury
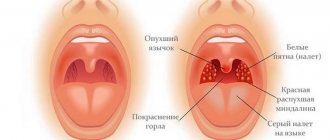
The initial diagnosis of a bruise can be carried out independently. To do this, you need to examine the mammary glands for the presence of lumps and swellings. You need to carefully check every centimeter of the breast and armpit with your fingers.
It is important to pay attention to the presence of the following changes: compaction, swelling, pronounced venous network, depression of the nipple, severe pain when pressed with a finger.
If at least one of the symptoms is present, you need to contact a specialist.
Ultrasound
An experienced mammologist will conduct a visual examination and prescribe a series of studies, which includes an ultrasound of the breast. This examination is also prescribed if a woman has hit her chest and is experiencing pain, but the doctor’s palpation does not reveal anything. Ultrasound easily reveals recent hematomas that have a homogeneous echo-negative structure, their location, size, and also allows you to detect vascular ruptures or damage to the ducts. Information about the hematoma not only facilitates the prescription of an accurate method of therapy, but also allows us to anticipate the possible formation of a capsule around the hematoma.
Mammography and other methods

There are additional examination methods that significantly expand the picture of the development and consequences of chest contusion:
Mammography is an X-ray of the breast and supraclavicular and axillary lymph nodes. it allows you to identify cystic neoplasms, benign and malignant tumors, anywhere in the breast.
Radiothermometry - analyzes the temperature level in different areas of the chest. This procedure helps determine the presence of inflammation in the deep layers of tissue, and also identifies malignant tumors and allows you to evaluate the effectiveness of the treatment.
MRI of the breast - visualizes each layer and reveals the exact location of inflammation or neoplasm, its nature, the likelihood of metastases, and ruptures or expansion of the milk ducts.
Medications
“Any hormonal medications—especially birth control—can cause breast pain because you are providing the body with a different dose of hormones than what your body normally receives,” says Dr. Dardik. Other medications that may cause similar pain include medications to lower blood pressure, hair loss medications, or to treat acne. Plus, some psychotropic medications have chest pain as a potential side effect.
Causes of chest injury
Breast injuries are divided into open and closed. The first type includes stab wounds, cuts, gunshot wounds, various bites and burns. Such damage not only leads to hematomas, but also creates tissue damage that requires antibacterial treatment to prevent infections.

Closed injuries involve maintaining the integrity of the skin, but the development of a hematoma. There are:
- premammary bruise - superficial hematoma;
- intramammary bruise - damage to adipose tissue, which leads to swelling and a purple tint;
- retromammary contusion - damage to the cellular space behind the mammary gland.
The causes of bruises can be associated with household injuries - a fall, a blow to a blunt object, damage during active games with a child. They can often be found in various sports involving a ball, puck, martial arts and sports equipment. Also, a large percentage of bruises occur in accidents, sometimes accompanied by rib fractures. Unfortunately, a woman runs the risk of getting a blow to the chest in any of the above situations, and in some cases this leads to bruises and other damage.
Uncomfortable bra
“A tight-fitting bra can certainly cause breast pain,” warns Raquel Dardik. “This is often due to hard underwires or a cup that is too narrow.” At the same time, uncomfortable underwear can provoke pain, regardless of the size of your bust. However, the expert notes that this is more common for girls with large breasts or those who lead an active lifestyle. That's why it's important to choose bralettes and push-up bras, especially when it comes to daily wear.
Milk stagnation
Sometimes the breasts are not completely emptied, which is usually due to the baby not latching frequently enough or due to an incorrect feeding position. In this case, pain, tension in the breast, hardening and redness may appear - this is how stagnation of milk makes itself known. If you are also suffering from the flu, severe fatigue or general malaise, then it’s time to go to bed. Contact your midwife right away to prevent milk stagnation from developing into mastitis or even a breast abscess.
The first therapeutic measures include frequently putting the baby to the breast - best in a position in which his chin is facing the sore spot.
If the baby is not hungry or does not suck well due to a runny nose, it is necessary to express milk using a breast pump.
Breast massage
Perhaps you don’t have a breast pump at hand, then massage will help you with pain and lumps.
They do it like this:
- Soak a clean gauze diaper in warm water, wring it out and apply it to your chest for about 5 minutes. Then start the massage. The main technique consists of circular movements, which are performed with the pads of the middle and index fingers. Start from the bottom, at the very base of the chest, and gradually work your way around the entire chest. Continue the massage, using your fingers to describe a spiral that should end at the areola.
- Lean forward slightly and use your palm to smooth your breasts on all sides, from the base to the nipple. In this case, you can lightly hold your chest with your other hand.
- Pinch the areola, slightly away from its edge, between your thumb and forefinger. Roll the nipple with light pressure. To activate all the lobes, you will need to change the position of your fingers several times, moving them around the areola.
- After the massage, it's time to cool your breasts. Spread the cold cottage cheese (from the refrigerator) onto a damp crepe paper kitchen towel. Fold it lengthwise in the middle and wrap it in a damp gauze diaper folded in half, so that you get a kind of cuff. After this, wrap it around your breasts like a compress, leaving the nipple and areola uncovered.
- As soon as the curd is warm, remove the compress. For more than just one-time use, wet it again and place it between two plates. In this form, the compress can be stored in the refrigerator and reused within 48 hours.
Infection
Breast infections are most common among breastfeeding women, although they are not exclusive to breastfeeding women. Such infections usually form in the breast tissue - in particular, mastitis and mastopathy. If we are not talking about feeding, the cause of inflammation can be piercings, damage to breast tissue, and even a common cold. Symptoms may include localized pain in the area of infection, hardness in the area, redness and itching (in some cases, fever and nausea). Dr. Dardik advises in this case to consult a doctor, since only he can prescribe the correct treatment - with the help of antibiotics and hot compresses.
How dangerous bruises can be
If you do not seek medical help in a timely manner, the risk of complications increases. They involve a change in the shape and appearance of the mammary gland due to the formation of scars, a predisposition to the tumor process, and an expansion of the spectrum of inflammation.
Complications appear:
- Suppuration. If a violation of the integrity of the skin is complicated by the entry of pathogenic microflora into the wound, pus is formed. The inflammatory process is accompanied by an increase in body temperature - first at the local level, then at the general level. The site of injury becomes red, swollen, and painful to the touch. The optimal treatment is antibiotic therapy, the use of analgesics, diuretics (to relieve swelling). In 9 out of 10 cases, the problem area is drained for better drainage of purulent masses. In general, the therapeutic program corresponds to the treatment regimen for purulent mastitis.
- The transition of inflammation to other structures of the chest.
- Malignancy of mastopathy into a cancerous tumor is a condition in which nodular elements of a benign nature become malignant. The process takes varying amounts of time, but is always accompanied by clinical manifestations. Symptoms include nipple retraction, breast tenderness on palpation; blue or blackening of the areola and nipple.
Without diagnostic measures and without going to the doctor, the risk of developing the listed complications increases.
A chest bruise is a closed injury that develops in response to a blow, collision, fall, or pressure. The areas within which this can happen are varied: from a traffic accident to an everyday fall from a height (for example, from a ladder during repairs). The damaged area turns red, becomes hard, compacted, which indicates the development of the pathological process and its main manifestation - hematoma. The optimal tactic to prevent the occurrence of complications is to consult a doctor.
Workout
In addition to the fact that your sports bra can pinch your breasts and cause pain, the workout itself can also be a source of pain. “There are two types of muscles responsible for chest pain,” says Raquel Dardik. - Firstly, these are the pectoral muscles, which are located below the chest and are worked in workouts such as the bench press. Secondly, these are small muscles between the ribs that cause local pain in the chest area.” The expert notes that in the first case, rest, ice and a mild painkiller (in extreme cases) will help you, in the second - time, since very soon the pain will go away on its own.
Cracked nipples
Feeding a baby with sore nipples is extremely painful. In addition, irritations and cracks pave the way for breastfeeding or thrush, so you need to do everything possible to avoid damage.
The following measures are recommended as prevention:
- Each time the baby attaches to the breast, he should also grasp a significant part of the areola with his mouth along with the nipple.
- To stop feeding, you must first eliminate the vacuum in the baby's mouth.
- Feeding should be done in a variety of positions.
- Use a few drops of breast milk to care for your nipples. After lubricating your nipples after feeding, let them air dry.
- Change your bra pads after each feeding.
If the nipples are already damaged, remedies such as:
- rubbing in lanolin;
- red light: after feeding, sit bare-chested at a sufficient distance from the lamp, sit for 20 minutes;
- nipple caps (until they heal);
- lots of fresh air for the chest.
• Problem No. 5: MOM GOT ILL
A mother who often feels unwell believes that she can no longer breastfeed her baby and switches to artificial feeding. In fact, most mother's diseases are not a contraindication for breastfeeding. You can safely do this if you have the flu, ARVI, or indigestion.
- Is breastfeeding allowed at fever?

This question puzzles almost every mother who is faced with this problem. Firstly, you already know that the temperature rises with lactostasis and mastitis, and with them you can continue to feed the baby. If the cause of fever is these diseases, then frequent and active breastfeeding is simply necessary, since it is the main means of solving this problem.
Secondly, modern doctors insist: breastfeeding at a temperature caused by some disease not related to breastfeeding is not only possible, but even useful! Antibodies enter the baby's body through mother's breast milk, which increase its resistance to this disease. This is a kind of vaccination, but without the virus, but immediately with agents of immunity against it. By stopping breastfeeding, you put your baby at even greater risk of contracting a cold or flu from you.
And if you need to take medications, just ask your doctor to select medications that are compatible with feeding.
However, if you urgently need to take medications that are not recommended during breastfeeding, then you will have to interrupt breastfeeding at a fever for the duration of treatment - but only for this time! When the course of treatment is completed, breastfeeding can be resumed. During treatment, feed the baby from a supply of previously expressed frozen milk, or switch to the formula that your pediatrician recommends. The latter, of course, is less acceptable, since after transferring the baby back to breastfeeding, it may be problematic.
To ensure that your baby safely returns to breastfeeding after a forced break, and that you do not have problems during breastfeeding, follow these recommendations:
- 1. Try to give your baby expressed milk or formula from a syringe, from a spoon, or feed from a cup - this way you will reduce the likelihood that your baby will “forget” how to suck on his mother’s breast (it is well known that infants have an internal need to suck the breast, and not in the milk itself);
- 2. In between feedings, you can give your baby a pacifier so that he satisfies his need for sucking;
- 3. While undergoing treatment, pump regularly - during the day about once every 2-3 hours, and at night 1-2 times between 3 and 8 o'clock in the morning. This is necessary to maintain lactation, and in addition, it will avoid stagnation of milk in the breast.
- 4. Find out from your doctor exactly how long after you stop taking the drug you can start feeding your baby.
When the course of treatment is over, you will finally be able to put your baby to your breast again. To make sure that there is enough milk after treatment, count the wet diapers 2-3 days after returning to breastfeeding (see their number below).
Top