Breastfeeding is not only about moments filled with happiness and togetherness with your baby. Often there are many troubles associated with lactation: cracks, lack of milk or, conversely, hyperlactation. One of these problems may be the formation of lumps in the mammary gland in a nursing mother. In addition to pain and discomfort, they can lead to serious complications.
What it is
Most often, lumps in the breast that occur during feeding are lactostasis. This is a stagnant formation that occurs when the milk duct is blocked and the lobe cannot be cleared of milk.
In itself, this nuisance does not pose any threat to the mother or baby, and it is quite common. But it is imperative to get rid of lactostasis in a short time, since the advanced form leads to the formation of mastitis. Purulent mastitis, which is subject to surgical intervention, is especially dangerous.
Causes of seals
Most breastfeeding women are faced with the problem of lumps forming, which turns feeding their baby into agony.
Seals form in one or two mammary glands at once. Certain sections of the ducts expand, and the speed of fluid passage to the nipple decreases. With increased milk density, stagnation occurs and a fat plug may form. The pain arises from the pressure of the milk, which stretches the walls of the ducts. The medical name for the phenomenon is lactostasis. There are different reasons for the occurrence of compactions:
- Spasm of the mammary duct in certain areas. A similar phenomenon follows after experiencing stressful situations. The cause of the spasm is hypothermia. Be sure to completely eliminate negative factors.
- Disturbances in the process of expressing milk. The more milk is expressed, more of it remains again. Lactation is a reflex process that cannot be controlled. With a large supply of milk, the ducts do not have time to distribute throughout the entire mammary gland in a timely manner, and areas of fluid stagnation are formed.
- Increased fat content. The cause of the phenomenon is the woman’s insufficient fluid intake, especially in the summer. Fatty milk forms plugs.
- Incorrect attachment of the baby during feeding. It is impossible to keep the child in one position, since the emptying of the breast occurs unevenly.
- Long breaks between feedings. According to previous standards, the baby should have been fed every three hours during the day. Such statements are not relevant today. The mother's milk reflexively begins to flow when the baby begins to cry. Don't put off feeding.
- Various types of chest bruises lead to the formation of painful lumps. It is important to protect the mammary glands from damage.
Symptoms
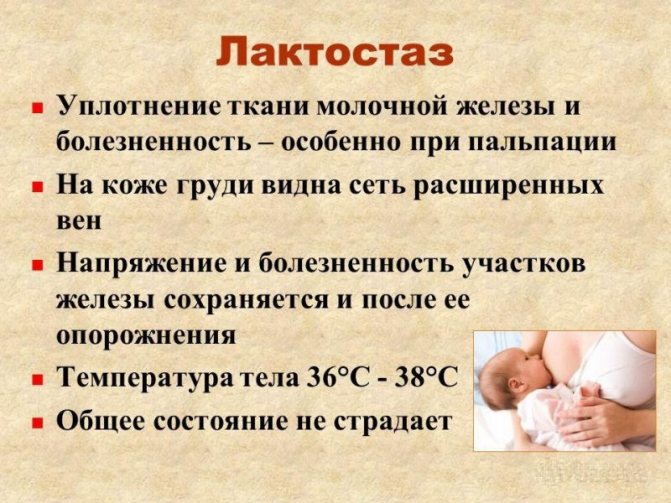
Symptoms of lactostasis manifest themselves in a fairly noticeable way:
- soreness;
- the presence of lumps in the breasts during lactation, which may disappear after a massage;
- uneven flow of milk from a painful breast;
- increase in breast volume - due to the presence of a large volume of milk in the breast;
- increase in body temperature - up to 40 degrees, occurs with advanced lactostasis;
- swelling and redness - occurs above the site of compaction and indicates that inflammation is occurring in the mammary gland.
Postpartum mastitis
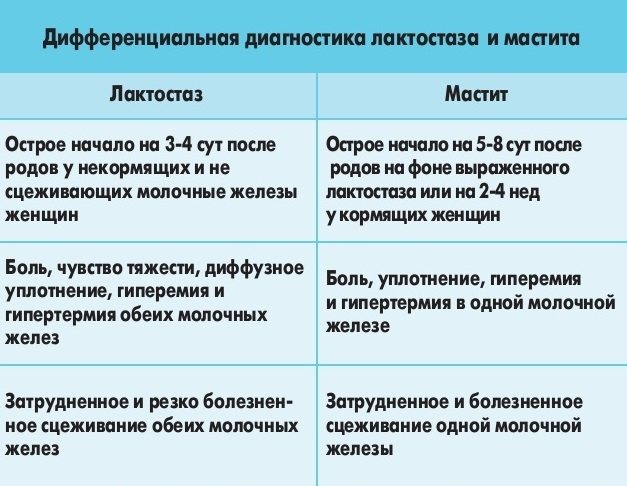
When the breasts become “stony”, feeding is painful, and the baby receives less and less milk, they speak of stagnation in the mammary gland. But if a sharp increase in temperature, chills, and the presence of softening spots in the center of the lumps are added to the above symptoms, the development of postpartum (lactation) mastitis should be suspected.
Most often, postpartum mastitis develops against the background of lactostasis (mastitis occurs in 4-11% of women). But clinically it happens that mastitis is not always preceded by a lump in the mammary gland. During breastfeeding, women (especially first-time mothers) often suffer trauma to the mammary gland, especially the nipple area. The cracks that appear are the gateway to infection, which, if hygiene rules are not followed, can easily get into the ducts of the gland. Thus, even without lactostasis it is possible (although rare) to develop lactation mastitis.
Causes of lactation mastitis
Postpartum (lactation) mastitis develops against the background of lactostasis (milk stagnation) when an infection is attached. The most common infectious agent is Staphylococcus aureus.

During the period after childbirth, a woman’s body is especially weakened. Therefore, failure to comply with hygiene rules, trauma to the breast as a result of improper feeding techniques, or the presence of endogenous (within the body) foci of infection increase the likelihood of developing mastitis. And if its first stage - serous - can be cured using therapeutic non-invasive methods, then in the second stage (infiltrative, purulent) in most cases they resort to surgical treatment (opening the abscess).
Treatment of mastitis at serous and purulent stages
During treatment for lactation mastitis, a woman should stop breastfeeding. Treatment of postpartum mastitis at the serous stage is as follows:
- Suppression of lactation.
- Compresses on the mammary gland (with butadione ointment, semi-alcohol).
- Physiotherapy on 2-3 days from the start of treatment (ultrasound, ultraviolet radiation).
- Antibiotic therapy.
- Immunomodulators.
- Desensitizing therapy (mainly histamine blockers).
The main method of treating purulent mastitis is opening the abscess. Most often, this operation is performed under anesthesia. But for small amounts of inflammation, local anesthesia can also be used. In addition to surgical intervention, women with purulent postpartum mastitis are prescribed broad-spectrum intramuscular antibiotics and immunomodulatory therapy.
Causes
Incorrect actions of the mother or the characteristics of the baby lead to the formation of compaction in the mammary glands during feeding. There are many reasons that cause lactostasis, but they all boil down to the fact that milk does not come out of some parts of the breast.
This is facilitated by:
- improper feeding of the baby;
- increased lactation, when too much milk is produced that the baby is not able to eat;
- the baby does not suckle actively;
- introduction of complementary foods, which significantly reduces the time the baby spends at the breast;
- uncomfortable posture during night sleep;
- blockage of the milk duct, which occurs due to cracked nipples or very fatty milk;
- incorrect posture when feeding or supporting the breast with your hand, in which some lobules of the mammary gland are pinched and are not emptied.
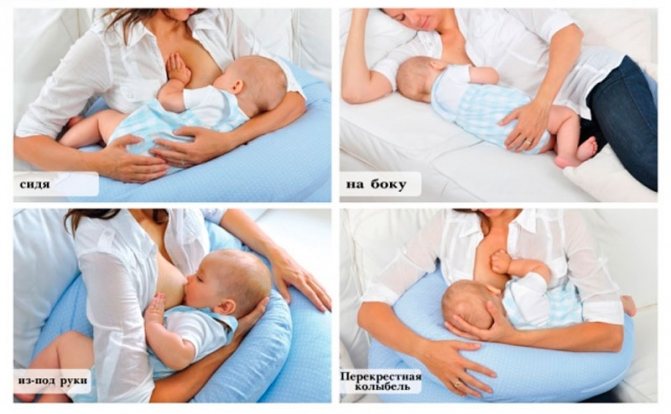
One of the common causes of breast lumps during breastfeeding is a monotonous feeding position. For example, the largest axillary lobe is poorly released from milk when the baby takes the breast in a standard “sitting” position. If the blockage occurs in the center of the upper part of the breast, then, most likely, the mother, while feeding the baby, holds the breast so that the nipple is pinched on top with the index finger, and on the bottom with the middle finger.

A separate painful lump has appeared in the chest - what is it?
This blockage of the milk duct (or several ducts) by a drop of milk fat is called lactostasis. In the first 1.5 months after birth, it may be accompanied by an increase in temperature. The main reason is errors in the organization of feeding the child and/or disturbances in the emotional balance of the mother, which provoke disruptions in the mechanisms of prolactin and oxytocin.
There are situations when lactostasis goes away on its own with more frequent application to the sore breast, but at the same time it periodically repeats if the mother does not know her mistakes and no one helps her correct them. There are complex lactostases that require immediate help to prevent complications such as mastitis. The mother needs help to establish a feeding rhythm, choose the most suitable feeding position in order to improve the drainage of the compacted area, monitor the quality of sucking and correct it if necessary. If this is done within 12 hours after the onset of stagnation, then lactostasis can be dealt with instantly. If more time has passed, then recovery will take longer.
I would like to say that compresses hardly help with lactostasis. To squeeze out a blood clot that has created a blocked duct, mechanical pressure is especially important - frequent sucking in the correct position and a specially selected position. The pose is selected depending on the location of the stagnation. Poor duct drainage is also associated with the fact that the baby is fed in the same position. For example, in the standard “sitting” position, the axillary lobe, the largest and with convoluted ducts, empties the worst. Therefore, the simplest action to prevent or eliminate stagnation of milk in the axillary lobes is to sometimes put the baby “from under the arm” (the mother sits, and the baby lies on a pillow with his head at the chest, and his butt and legs behind the mother’s back). In this position, the baby sucks everything perfectly.
The location of lactostasis on top “in the center” is typical for those cases when the mother holds the breast with “scissors” during feeding - the nipple is between the index and middle fingers, the index finger is pressed into the breast. This way the breast can neither be supported nor fed. It should be supported with the whole hand - the thumb on top, the rest under the chest. But it is best if the baby holds the breast on his own, without the help of his mother.
If a woman has large and heavy breasts, one of the reasons for the formation of lactostasis is sleeping at night in an uncomfortable position. Try to sleep on your stomach with a comfortable pillow more often. Then, during strong hot flashes, the milk will simply flow out and not stagnate.
Various troubles, including lactostasis, usually happen to those mothers who ignore such a concept as properly organized breastfeeding.
You are at risk of lactostasis if you: accumulate large portions of milk, do not feed on demand, supplement with liquid before or shortly before feeding, apply to the breast in the same position all the time. However, lactostasis is a mysterious and unpredictable thing. Sometimes it appears out of nowhere. However, if the child actively sucks on the affected breast, it resolves within 1-2 days without special measures. The main thing is not to panic and, of course, not to stop feeding in fear.
Symptoms of lactostasis Body temperature rises to high numbers (30-40 ° C). The mammary gland increases in volume, it is painful when palpated, and areas of compaction may appear. There is no swelling and redness of the skin characteristic of inflammation (mastitis).
Advanced lactostasis, which the mother cannot cope with for more than 3 days, is very dangerous, because... may progress to mastitis. Equally dangerous is the mother’s incorrect actions during lactostasis.
What NOT to do if lactostasis occurs: stop feeding the affected breast, even if there is a very high temperature, leave the painful lump unattended during the night break. If there is no guarantee that the baby will wake up on his own in 2-3 hours, it is better for the mother to use an alarm clock to provoke the baby to suckle every 2 hours.
Possible complications
The main complication that can result from stagnation of milk with hardening in the mammary gland in a nursing woman is mastitis, and especially purulent one. It is a consequence of bacteria entering the breast tissue. This can happen if there are chronic infectious diseases or damage to the skin in the nipple area.
In most cases, a woman’s immune system copes with bacteria, but stagnation of milk in the ducts is an excellent breeding ground for pathogenic microorganisms. If the lump cannot be broken for a long time - more than 3 days, and the temperature rises, the chest swells and turns red in places, most likely, the inflammatory process is already underway.
In this case, you should immediately consult a doctor, since advanced purulent mastitis is an indication for surgical intervention. How to remove lumps in the chest? If you consult a specialist in time, it is possible to remove inflammation using ultrasound and other physiotherapeutic methods.
Complex treatment
Treatment of lumps in the sternum in women that arise during breastfeeding requires an integrated approach. The fight against lactostasis should begin immediately after its detection. After 12 hours, this is much more difficult to do, the woman’s well-being may worsen, and the likelihood of an infectious process increases significantly.
If there is no temperature yet and the mother’s condition is satisfactory, a number of measures can be taken to help eliminate the bumps. To do this, you need to clear the stagnation and completely empty the breast lobe of milk. How to get rid of lumps in the chest?

Proper preparation
Before taking direct measures to get rid of balls in the chest during breastfeeding, it is necessary to prepare the chest. The most preferable is a warm shower or compress for a few minutes, after which the area of the lump is lightly kneaded until it becomes softer.
Under no circumstances should these measures be resorted to in the case of advanced lactostasis and elevated temperature, since it is not known at what stage of inflammation the damaged lobule of the mammary gland is located.

Frequent applications
The best way to deal with such a problem is to try to get the child to resolve the stagnation. If you apply the baby more often to the affected breast at the beginning of lactostasis, there is a high probability that he will cope with it. Before feeding, it is advisable to express a little milk - this will help the baby suck more actively.
In order for the sucking process to be most effective, an important rule should be observed - the area of compaction in the chest during feeding should be under the child’s lower jaw. In the case where the feeding position is extremely uncomfortable, for example, the upper part of the chest is affected, you can lie down with the baby on the bed in a certain way.
Compresses
They help soften the lump in the mammary gland during feeding, and also somewhat reduce pain. Depending on the compress itself, it may have an anti-inflammatory and antiseptic effect.
The most effective and easiest to use is a napkin or towel moistened with warm water, which is applied to the sore chest. It is kept until it cools down. A cabbage compress is very common and quite effective for breast diseases. The cabbage leaf is beaten until the juice is released and applied to the sore spot. It is believed to help with inflammatory diseases of the mammary gland.

Pumping
If your baby’s help fails to dissolve a lump in the mammary gland while breastfeeding, you can try to do it yourself.
To do this correctly, you need to follow a certain technique that will not make the situation worse. If lactostasis has already occurred, and there is an excess of milk, you should express a little yourself after finishing feeding so that it does not stagnate in the breast for a long time.

Feeding for lactostasis

Many women, when lactostasis occurs, are afraid to continue breastfeeding, believing that milk becomes harmful to the baby.
Doctors say in this regard that if the period of lactostasis does not exceed three days, this does not pose any threat, but in any case, this phenomenon must be eliminated as soon as possible. During breastfeeding with lactostasis, you must follow several simple rules:
- Ensure the correct position of the baby - his chin should always be directed exactly in the direction where the lump appeared in the mammary gland.
- The baby should be put to the breast at least every two hours.
- When starting to feed, it is necessary to warm up the mammary glands. For these purposes, you can use a warm compress or shower.
- If the lumps are very pronounced, it is recommended to express the milk a little - in some cases, this procedure will help completely eliminate the blockage of the duct and restore normal milk flow.
- When expressing breast milk, special care must be taken not to injure the milk ducts. You shouldn't do this too often. The optimal schedule is once every three days.
- After each feeding, it is recommended to apply cool compresses to the affected breast for about 10-15 minutes.
For compresses, you can use mineral water or decoctions of medicinal herbs. Substances such as alcohol and camphor are contraindicated in this case, since they can only aggravate the irritation and inflammatory process.
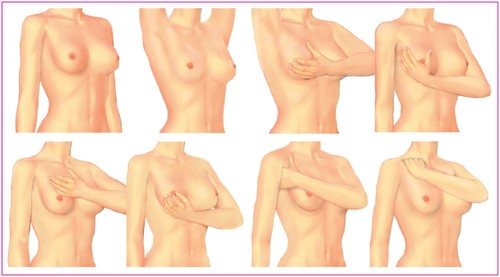
How to strain correctly
The technique of straining stagnation is not complicated. It should be remembered that this procedure should not cause significant pain. Excessive pressure and active massage should also be avoided. All movements should be soft and smooth.
Let's look at how to break up lumps when breastfeeding:
- Before pumping, prepare the breasts with heat and a little massage, and wash your hands and mammary glands well.
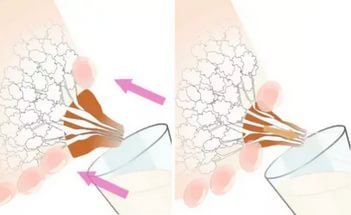
- The chest should be grasped as follows: the thumb is opposed to the other 4 fingers. For example, the thumb is on the top of the chest, and the other four support the chest from below.
- Your fingers should be near the edge of the areola. Pressure is applied not to the lobules of the gland, but to the edge of the areola, while slightly pressing it into the chest.
- The lump in the breast during breastfeeding, which is located under the thumb, will be cleared.
- If milk is no longer released, you need to massage the clogged part of the breast a little more and try again.
- You should not focus only on working on the seal; it is better to express the entire breast.
After feeding or pumping, apply a cold compress to your breasts to reduce milk flow. For the same reason, it is better to reduce the amount of fluid you drink at this time.
What not to do
There are certain actions that should be avoided so as not to aggravate lactostasis and not provoke the development of mastitis:
- Alcohol compresses should not be used. They inhibit the production of the hormone oxytocin, which helps effectively remove milk from the mammary gland. The consequence is heavy milk production, the baby gets tired of sucking it and doesn’t get enough, and the likelihood that lactostasis will go away also decreases.
- Hot compresses are contraindicated, especially at high temperatures, when there is a high probability that mastitis has begun.
- Aggressive massage should not be used. Inexperienced or too active actions near the lump can further injure the mammary gland and form new lumps in the mammary glands. In addition, if suddenly mastitis has already begun, pressing on the bag of pus can lead to its rupture.