Painkillers during breastfeeding should be harmless to mother and baby. If the drug passes into breast milk, it can cause unexpected effects in the baby.
All analgesic tablets have side effects. Recommended for use strictly in certain dosages.
When prescribing painkillers, pediatricians recommend temporarily stopping breastfeeding. Foreign experiences show that a sudden refusal to feed is harmful not only for the child, but also for the young woman.
Let's consider all the subtleties and nuances of prescribing analgesics during breastfeeding.
Painkillers during breastfeeding
Doctors believe that the safest painkillers are paracetamol. The drug does not pass into breast milk, but penetrates the placenta. No side effects on the fetus were identified. Eliminates moderate pain, has an anti-inflammatory effect. Fervex and Efferalgan are made from paracetamol and are recommended in the second trimester of pregnancy.
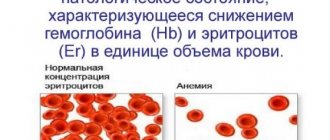
Analgin is prohibited during breastfeeding. Such tablets are excluded from the available list in Europe due to serious complications. If the drug enters the child’s blood, it thins and leads to a decrease in hemoglobin concentration.
No-shpa and Riabal are antispasmodic tablets. Eliminate pain by relaxing muscle fibers around blood vessels and intestines.
Nonsteroidal anti-inflammatory drugs (Voltaren, diclofenac) are taken with extreme caution. There are no clinical studies regarding their accumulation in breast milk. Dicloberl is used to relieve back pain when carrying a child.
In case of moderate pain syndrome, it is rational to use not systemic drugs, but local dosage forms - gels, ointments.
Contraindications and restrictions
The drug is contraindicated in the following diseases and conditions:
- Intolerance to Panadol components.
- Increased concentration of bilirubin in the blood.
- Glucose-6-phosphate dehydrogenase deficiency.
- Severe dysfunction of the liver and kidneys.
- Hematopoietic disorders (anemia, leukopenia).
- Children under 6 years of age (soluble tablets).
- Patients under 12 years of age (tablets with a concentration of 500).
- Alcohol addiction.
If the rules of use are violated or there are contraindications, the medication provokes negative phenomena:
- nausea, vomiting, epigastric pain;
- anemia, decreased concentration of platelets, leukocytes;
- skin rash, itching, urticaria, anaphylaxis;
- decreased blood glucose concentration, hypoglycemic coma, bronchospasm, etc.
Panadol is not contraindicated during lactation.
What painkillers can you take while breastfeeding?
What painkillers do doctors allow a breastfeeding woman to take:
- Ketoprofen;
The main feature of using non-steroidal anti-inflammatory tablets for pain is a one-time use.
Pregnant and breastfeeding women are confident that it is better to abstain from medications during these important periods of life. This is true. But situations arise when one-time or long-term medication cannot be avoided. By what criteria is their toxicity assessed and what can be treated during lactation.
Emergency or planned prescriptions of medications may be associated with exacerbation of chronic diseases, the development of acute pathologies or postpartum complications.
In each case, therapists, obstetricians and pediatricians assess the degree of toxicity, the level of entry into milk and the possible risk of negative effects on the baby’s body.
Many developments in the pharmaceutical industry do not undergo testing and clinical trials in pregnant and lactating groups. There are few or no reliable, adequate studies. The list of studied means is quite short. But one thing is clear: if the drug is absorbed and distributed in the body fluids, then to a greater or lesser extent it passes into breast milk.
Therefore, in most annotations for drugs, manufacturers write that use should be careful, for special purposes, without exceeding the dosage.
The degree of risk of any drug is assessed according to several criteria:
- Toxicity.
- The true amount of the substance that enters the baby’s body with milk.
- Features of the influence on immature organs and systems of the newborn.
- The period of elimination of the drug from the child’s body.
- Possibility of allergic manifestations.
- Individual characteristics of mother and baby.
- Duration of taking the drug.
Most new drugs have a low degree of toxicity and are considered safe for nursing mothers. This also applies to external preparations: ointments, creams, drops and solutions. They are not absorbed into breast milk.
Antibacterial agents
Despite the fact that drugs of the penicillin, cephalosporin series and macrolides are approved for the treatment of nursing mothers with the wording in the annotation “usually not contraindicated”, in any case the question of the advisability of such treatment, calculation of dosages taking into account the condition of the mother and baby is required. Antibiotics from these groups can penetrate into milk only in negligibly small quantities. Average: 0.090% of a single dose for the patient.
There is a danger for babies after using antibacterial agents. They can cause:
- Allergic reactions.
- Imbalance of the gastrointestinal microflora with impaired production of vitamin K and D, and as a result - prothrombin deficiency.
During lactation the following are allowed:
- From macrolides Erythromycin. The rest Sumamed, Vilprofen, and other drugs from this group are contraindicated.
- Aminoglycosides Neomycin, Kanamycin, Amikacin.
The latter are more toxic, and they are prescribed in special cases: patients who have been diagnosed with meningitis, sepsis, peritonitis or abscess of internal organs.
Completely contraindicated:
- Fluoroquinolone group (Norfloxacin Ciprofloxacin Ofloxacin). This series of antibacterial drugs causes disturbances in the formation of bone and cartilage structures during growth.
- Group of tetracyclines (Tetracycline, Doxycycline). Gives a high degree of hepatotoxicity.
- Nitromidazoles (Metronidazole, Tinidazole). Causes dyspeptic disorders.
- Sulfonamides (Streptotsid, Norsulfazole). They depress the liver, provoke pathological jaundice in the baby, and inhibit hematopoiesis.
- Biseptol and its analogues. Inhibits bone marrow functions.
Lines of antimycotic and antiviral agents for absorption and action through breast milk have not been fully studied, so their use requires stopping feeding.
If a woman has stopped breastfeeding and completed a course of antibacterial therapy, she should resume it only when all metabolites have been eliminated from the body.
Analgesics, antipyretics, anesthetics
During the postpartum period and in the first months of lactation, a woman experiences enormous stress, hormonal changes, and exacerbation of chronic diseases. Therefore, she is often worried about pain, inflammation, and fever.
To relieve these symptoms during lactation, non-steroidal anti-inflammatory drugs based on two active ingredients are allowed: paracetamol and ibuprofen. They are universal and are used for headaches, muscle, groin, dental and other types of pain.
Despite the fact that the effect of PVNS has not been fully studied, it is believed that a single dose is not capable of producing a toxic effect on the infant’s body. The recommended dosage for women in this category is no more than three doses per day.
Paracetamol as an active substance is included in the list of approved drugs:
- Panadol.
- Efferalgan.
- Stimol.
Based on ibuprofen, the following are allowed:
- Nurofen.
- Advil.
- Burana.
A woman should take any of the drugs from these groups immediately after breastfeeding. This is necessary so that by the next feeding the drug has gone through a full metabolic cycle and lost its pharmacological activity (toxicity).
Analgesics, or painkillers based on metamizole sodium, are prohibited. This list includes trade names: Analgin, Sedaglin, Tempalgin, Pentalgin, Baralgin.
The main active component of the drugs passes into breast milk and negatively affects the hematopoietic and urinary system of the baby. In addition, metamizole-based analgesics include codeine or caffeine, which can cause dyspepsia and neurological disorders.
Acetylsalicylic acid (Aspirin) is allowed during breastfeeding in a single dose.
During lactation, women are allowed local injections of the latest generation of anesthetics:
- Dicaina.
- Ultracaine (Articaine).
- Ubistezina
- Melivacaina (Scandonesta).
For breastfeeding, Novocaine and Lidocaine are contraindicated.
Description of dosage forms
The tablet form of Panadol differs only in the concentration of paracetamol (200, 350, 500 mg). Rectal suppositories also differ in the amount of active ingredient: 50, 100, 125, 250 and 500 mg. Syrup and oral suspension are intended for the youngest patients. In addition, Panadol is available in soluble tablets.
As mentioned earlier, the active component of the drug is paracetamol; the dosage forms differ only in additional substances:
Pills:
- starch;
- octadecanoic acid;
- milk sugar;
- calcium stearate;
- gelatin;
- povidone;
- sodium starch glycolate.
Rectal suppositories:
- hard fat.
Suspension:
- water;
- aromatic additives;
- dye;
- glycerol;
- sorbitol;
- xanthan gum.
The most popular dosage forms are described above.
After penetration into the body, paracetamol affects the center of pain and thermoregulation, which is located in the brain. Panadol inhibits the production of prostaglandins, which are responsible for fever and pain.
The therapeutic effect appears 40–60 minutes after administration. After oral administration, its components are quickly absorbed into the bloodstream through the intestines. The remaining medication is excreted in the urine.
Panadol is used to relieve pain of various natures:
- For headaches.
- For muscle, joint, rheumatic pain, neuralgia.
- For painful periods.
- For toothache.
In addition, the medication is used to relieve the characteristic symptoms of influenza: fever, headache, body aches.
Nootropics, antidepressants
Drugs from the group of neurometabolic stimulants are indicated during breastfeeding. The list of permitted ones includes:
- Stugeron.
- Nootropil.
- Vinpocetine.
- Glycine.
- Pramiracetam.
- Bifren.
- Cerebrolysin.
- Piracetam.
In the treatment of postpartum depression, only one of the groups is prescribed exclusively for special indications: selective serotonin inhibitors (Sertalin, Fluoxetine).
Tablets and injections based on phenobarbital, codeine and caffeine are prohibited.
Groups of drugs without contraindications
Women during lactation are allowed to systematically take the antihypertensive drug Methyldopa and its analogues Dopanol, Dopegit.
In severe cases of hypertension, Capropril, Enalapril can be prescribed in combination with the diuretics Veroshpiron or Hydrochlorothiazide.
The list of medications allowed during breastfeeding includes:
- Choleretic agents, enzymes, antienzymes: Festal, Allohol, Cholenzym, Enzistal, Oraza, Pepfiz.
- Preparations of enveloping and adsorbing action: Enterosgel, Polyphepan, Activated Carbon, Carbolene, Tanalbin.
- Inhaled corticosteroids for bronchial asthma.
- Hormonal agents for the treatment of autoimmune pathologies.
- New generation monophasic oral contraceptives based on desogestrel and levonorgestrel: Microlut, Lactinet.
- Short-term antihistamines: Cetirizine, Loratadine. First generation drugs (Suprastin, Tavegil) are not prescribed.
- Plant-based laxatives Guttalax and Regulax are allowed, but in moderate dosages. Bisacodyl is not recommended.
- Multivitamins and minerals.
Every woman should know that the safety and toxicity of drugs directly depends on the age and status of the baby. For example, in the weak, premature and in the first two months of a newborn’s life, the process of absorption and excretion of drugs does not occur at the same speed as in older and heavier children. Therefore, dosages, course duration, type and form of medication should be discussed exclusively with a doctor. Only a specialist will suggest the optimal dosage regimen and thereby reduce the risks of negative effects on the child. And this is an axiom that is not discussed.
Breastfeeding mothers often ask what pills a nursing mother can take. In Soviet times, it was believed that you should not take medications while breastfeeding. However, later WHO conducted a number of studies. Research results have shown that most medications can be taken while the mother is breastfeeding. A small part of the drug passes into mother's milk. The drug reaches its maximum concentration in milk no earlier than two to three hours after administration, and then is gradually eliminated from the body. Therefore, it is simply enough to correctly calculate the safe time between taking the pill and feeding.
What can be replaced
The modern range of medicines based on paracetamol is very wide. And most of them (those that do not contain other components contraindicated for pregnant women) can be used to treat pregnant women as indicated.
Table: popular structural analogues of Panadol prescribed to pregnant women
| Drug name | Paracetamol concentration | Indications for use | Contraindications |
| Paracetamol |
|
|
|
| Efferalgan |
|
| |
| Tsefekon D | 1 rectal suppository - 0.05, 0.1 or 0.25 g | Hypersensitivity to the components of the drug | |
| Perfalgan | 1 ml solution for infusion - 0.01 g |
|
Photo gallery: paracetamol-based drugs used in any trimester of pregnancy
Perfalgan is a paracetamol-based drug, presented in the form of a solution for infusion

Cefekon D - popular and inexpensive paracetamol-based rectal suppositories for children

Efferalgan is also available in the popular form of effervescent tablets
Paracetamol is the cheapest analogue of Panadol
Among the less popular structural analogs of Panadol that can be used during pregnancy are the following drugs: Acamol Teva, Aldolor, Apap, Acetaminophen, Daleron, Ifimol, Calpol, Xumapar, Lupocet, Mexalen, Pamol, Prohodol, Sanidol, Strimol, Tylenol, Febricet.
What pills can a nursing mother take?
Before taking any pill while breastfeeding, you should consult your doctor and carefully read the instructions. For acute pain (toothache, headache), you can take Ketarol, Calpol, Panadol. But tablets containing analgin cannot be taken while breastfeeding. Analgesics, penetrating into milk, disrupt the process of hematopoiesis, cause changes in kidney function, and also have a depressing effect on the infant’s nervous system. Aspirin should also not be abused. When taking the drug in large doses, its concentration in mother's milk increases, and this often leads to metabolic disorders in the baby.
Among drugs for high blood pressure, Capoten is considered the safest medicine for breastfeeding. The concentration of this drug in breast milk is the lowest among similar drugs.
If you have indigestion, among all the tablets during breastfeeding, the safest would be an activated carbon tablet. Anti-poisoning medications should be taken with extreme caution, but laxatives will not affect the child’s health in any way.
You can take tablets with antihistamine action while breastfeeding, but you must choose drugs with only one action.
Almost all drugs from the antidepressant group retain high concentrations in breast milk for a long time, so they can only be taken after prior consultation with a specialist. If you are excessively nervous and irritable, it is best to replace the pills during breastfeeding with herbal tea with a calming effect.
Possible side effects and contraindications
Long-term use of Panadol in large dosages has a toxic effect on the liver and kidneys. However, the doses used in the treatment of pregnant women and compliance with the safe duration of the course of treatment are guaranteed to protect the expectant mother from such hazardous health consequences. Possible side effects of the drug include:
- allergic reactions in the form of skin rashes, itching, Quincke's edema;
- nausea, pain in the epigastric region;
- renal colic;
- interstitial glomerulonephritis;
- aseptic pyuria;
- agranulocytosis;
- thrombocytopenia;
- sleep disorders - for Panadol Extra;
- rapid heartbeat (tachycardia) - for Panadol Extra.
Studies conducted in Britain have shown that the use of paracetamol in the second half of pregnancy significantly increases the risk of the child developing allergic reactions, asthma and respiratory disorders.
The list of contraindications for taking Panadol is as follows:
- severe kidney or liver dysfunction;
- epilepsy;
- glaucoma;
- arterial hypertension;
- hypersensitivity to the components of the drug;
- sleep disorders - for Panadol Extra.
Antibiotic treatment during breastfeeding
Treatment with antibiotics during breastfeeding has a negative impact on the baby's health. If possible, such treatment should be abandoned.
If a doctor has prescribed antibiotics for breastfeeding, it is better to take them immediately after feeding or during feeding. If the drug can harm the baby, then you can stop breastfeeding for a while or express the so-called “medicated” milk. Milk with the maximum concentration of the antibiotic must be expressed and discarded two to six hours after taking the drug, and after that the baby can be fed again.
All antibiotics are divided into several groups depending on the level of concentration in breast milk and the effect on the baby’s body. Prohibited antibiotics during breastfeeding include tetracyclines and sulfonamides. Taking these drugs can lead to disruption of the development of the child's organs and to toxic damage to the body.

The group of macrolides is not so dangerous, however, caution must be exercised when using antibiotics from this group. When prescribing these medications to the mother, the child is additionally prescribed medications for dysbiosis.
Penicillins, cephalosporins, aminoglycosides are most compatible with breastfeeding. However, the duration and dosage of these tablets during breastfeeding should only be determined by a doctor.
Paracetamol during breastfeeding
Paracetamol during breastfeeding will help to quickly reduce the temperature. Within half an hour after taking the drug, the mother will feel noticeable relief. Paracetamol helps with toothache and headache. This drug in tablets can be taken during breastfeeding for no longer than two to three days. The optimal dose of the drug is one tablet of the drug up to three to four times a day. These tablets should be taken when breastfeeding so that the feeding time does not coincide with the periods of maximum concentration of the drug in the blood plasma. When treating with paracetamol, you must follow all the rules and carefully monitor the baby’s well-being.
Hello everyone, my dear readers. Finally got around to writing this article. What medications can you take while breastfeeding? I made my first notes when I was breastfeeding my son and had a severe toothache. There was nothing at home except paracetamol and I went to the pharmacy. I asked the pharmacist to give me something for toothache. Of course, I said that I was feeding the child, which I later regretted very much. The answer was that I couldn’t do anything at all, they said take noshpa or paracetamol. They also scolded me for not thinking about the health of my child.
Of course, I was unpleasantly surprised by such unprofessionalism of the specialists. In the end, they finally sold me at least spasmalgon, but with great difficulty. Recently, there was a similar situation. I went to the pharmacy and asked for lozenges for a sore throat. But my belly can no longer be hidden. The girl refused to give me the ones I asked for and thought for about 10 minutes about what I could do. In the end, I said that I wasn’t taking it for myself and chose the drug myself in 30 seconds.
In fact, this is very serious, because statistics say that many women give up breastfeeding because they get sick and even doctors prescribe medications that are incompatible with breastfeeding. In such a situation, everyone suffers - the child for whom it is a lot of stress and, of course, the mother.
Of course, it’s better to live without drugs, it’s better for everyone. But situations are different, and if you are pregnant or breastfeeding, this does not mean at all that you should suffer from pain. On the contrary, your torment brings even more torment to the baby and in the end everyone suffers.
To begin with, I’ll tell you why this happens and why the annotations of almost all medications include contraindications for periods of breastfeeding and pregnancy.
Here is a certain company that produces medicines. In order to write to her that this drug is approved for breastfeeding, she needs to conduct clinical trials. And this, firstly, is very expensive, and secondly, it takes a long time, because some complications do not appear immediately, but several years after taking the drug . And in order not to take responsibility, they write that the drug is contraindicated during pregnancy and breastfeeding. And it’s cheap and you don’t have to take responsibility...
But there is an independent company that conducts such research, this is their main job, and this data is entered into special reference books, which lactation consultants are required to have and also available to doctors and pharmacists who do not sit on they are engaged in their education, improving their skills and attending various courses.
Here's information about the most common medications to help you. Use it for your health, spread the word, if you have questions, write in the comments. (using the reference book of the World Health Organization, Karpov’s reference book “Risk of using medications during pregnancy and lactation”,
Hale's reference book
“Medications and Mothers' Milk.”
Breastfeeding Pharmacology"). I most often use this reference book https://www.e-lactancia.org/ingles/inicio.asp It is very easy to use. detailed instructions.
I decided to make you a list of the most popular drugs that many of you have in your medicine cabinet and which are completely allowed for nursing mothers and which are allowed in small doses. So:
Panadol during lactation
Natalia Belyaeva. Nursing mothers often suffer from colds, which are accompanied by a fever. When the temperature rises from In addition, a lactating woman is not immune from pain of various origins: pain in the head, back, muscles, joints, neuralgia, etc.
Then the woman tries to find an effective drug that will eliminate pain, fever and will not harm the newborn. Panadol is one of the forms of the well-known Paracetamol. The medication normalizes temperature during heat, eliminates the inflammatory reaction and moderate pain.
The drug is produced in different pharmaceutical forms for adults and small patients. Women are interested in whether Panadol can be taken by a nursing mother. According to doctors, if certain rules are followed, the medication will eliminate unpleasant symptoms and will not harm the baby. The tablet form of Panadol differs only in the concentration of paracetamol, mg. Rectal suppositories also differ in the amount of active ingredient: 50, , , and mg. Syrup and oral suspension are intended for the youngest patients.
In addition, Panadol is available in soluble tablets. As mentioned earlier, the active component of the drug is paracetamol; the dosage forms differ only in additional substances: After penetration into the body, paracetamol affects the center of pain and thermoregulation, which is located in the brain. Panadol inhibits the production of prostaglandins, which are responsible for fever and pain.
The therapeutic effect appears 40 - 60 minutes after administration. After oral administration, its components are quickly absorbed into the bloodstream through the intestines.
The remaining medication is excreted in the urine. In addition, the medication is used to relieve the characteristic symptoms of influenza: fever, headache, body aches. Panadol tablets are swallowed and washed down with purified water, effervescent pills are dissolved in water. Rectal suppositories are inserted into the cleaned anus, and syrup is given from a spoon. The choice of pharmaceutical form, dosage, frequency, duration of use of the drug is determined by the attending physician. As the instructions say, patients over 12 years of age are prescribed from 0.
The medicine is used at intervals of 4 hours. Children from 6 to 12 years old take from 0. The maximum dose for adult patients is more than 4 mg of the drug, and for children - from 2 g. You should not take the medicine for more than 3 days in a row without the knowledge of the doctor. If symptoms do not disappear after this period of time, then stop taking Panadol and consult your doctor.
The drug is contraindicated in the following diseases and conditions:. If the rules of use are violated or there are contraindications, the medication provokes negative phenomena: If a lactating woman has a headache, toothache or fever, then she needs safe medications. Panadol can be taken during breastfeeding if absolutely necessary: if the temperature is higher. According to doctors, the drug is safe for mother and newborn if the dosage and other rules of administration are observed.
For breastfeeding, it is allowed to take tablets, a single dose - from to mg three times a day. The medicine is taken immediately after feeding, washed down with filtered water. Thus, Panadol during breastfeeding is an effective and moderately safe drug. Without the doctor's information, a woman can take the medicine once in a minimum dosage.
In other cases, the use of Panadol must be agreed with the doctor. Graduated from Krivoy Rog Medical College, specialty - pharmacy, experience in a pharmacy - 5 years. If the mother is sick Nursing mother October 19, Topics of articles Medicines. The drug is contraindicated in the following diseases and conditions: Intolerance to Panadol components. Increased concentration of bilirubin in the blood. Glucose phosphate dehydrogenase deficiency. Severe dysfunction of the liver and kidneys. Hematopoietic disorders: anemia, leukopenia.
Children under 6 years of age, soluble tablets. Patients under 12 years of age tablets with a concentration of Alcohol dependence. If the rules of use are violated or there are contraindications, the medication provokes negative phenomena: nausea, vomiting, epigastric pain; anemia, decreased concentration of platelets, leukocytes; skin rash, itching, urticaria, anaphylaxis; decreased blood glucose concentration, hypoglycemic coma, bronchospasm, etc.
Leave a comment Cancel reply Your email will not be published.
List of popular drugs:
- Ibuprofen is fully compatible
- Acetylsalicylic acid - compatible in a single dose
- Spasmalgon - can be taken in a single dose
- Citramon - can be taken in a single dose
- Ibuklin is fully compatible
- Ketoprofen is fully compatible
- Ketanov - fully compatible
- Analgin is prohibited for breastfeeding mothers
- Motilium - allowed for hepatitis B
- Aflubin - fully compatible
- Bioparox - fully compatible
- Acyclovir - fully compatible
- Novo-passit - allowed for breastfeeding, but with caution, choose a small dosage of the drug
- Caffeine - taken with great caution, not advisable
- Mezim - fully compatible
- Pancreatin is fully compatible
- Noshpa-fully compatible
- Voltaren - fully compatible
- Zyrtec - fully compatible
- Immune compatible, but with caution
- Immodium - fully compatible
- Claritin - fully compatible
- Lazolvan - fully compatible
- Ambroxol - fully compatible
- Sumamed is fully compatible
- Flucostat is fully compatible
- Ersefuril is fully compatible
- Enap-fully compatible
- Diclofenac - fully compatible
- Omeprozole - fully compatible
- Cefazolin - fully compatible
- Metronidazole is fully compatible
- Trichopolum is fully compatible
- Furazolidone is fully compatible
- Amoxiclav is fully compatible
- Doxycycline is compatible, but use with caution for no more than 3-4 weeks
- Ibuklin is fully compatible
- Cephalexin - fully compatible
- Smecta - fully compatible
- Activated carbon - fully compatible
- Prednisolone - fully compatible
- Pirantel - fully compatible
- Phenoborbital - fully compatible
- Phenytoin - fully compatible
- Amoxicillin - fully compatible
- Ampicillin - fully compatible
- Bicilin - fully compatible
- Ferruginous moth - fully compatible
- Folic acid - fully compatible
- Heparin - fully compatible
- Salicylic acid - fully compatible Miconazole - fully compatible Nystatin - fully compatible
Dear women, if the instructions for the drug say that breastfeeding should be discontinued while taking the drug, do not be alarmed! You just need to check the drug in one of the reference books that I wrote about above (there are also active links to help you) and if the medicine really cannot be used, then it can be replaced with an analogue with the help of a doctor or breastfeeding consultant. Almost every medicine has an analogue tested for compatibility with breastfeeding.
And I wish you to lead a healthy lifestyle and be healthy without drugs!
Best regards, Oksana Litvinova
My daughter was only a month old when lack of sleep, worries and numerous worries made themselves felt: I had a terrible headache. I bravely endured the whole day, remembering that taking medications and breastfeeding are incompatible things. When the headache did not go away by the end of the second day, I called a doctor I knew. It turned out that the pain I endured was much more harmful than the consequences of taking the pill.
Children's Panadol, Extra and other varieties
There are several varieties of Panadol, the possibility and safety of which pregnant women should use separately.
Panadol Extra is a drug that, in addition to paracetamol, contains another active component that enhances its effect - caffeine . Although the negative effect of large doses of this substance on the course of pregnancy is an indisputable fact today, the instructions for the drug do not list pregnancy as a contraindication, but only indicate the need to use it with caution. This is probably due to the low concentration of caffeine and the short-term or occasional need for treatment with Panadol in expectant mothers.
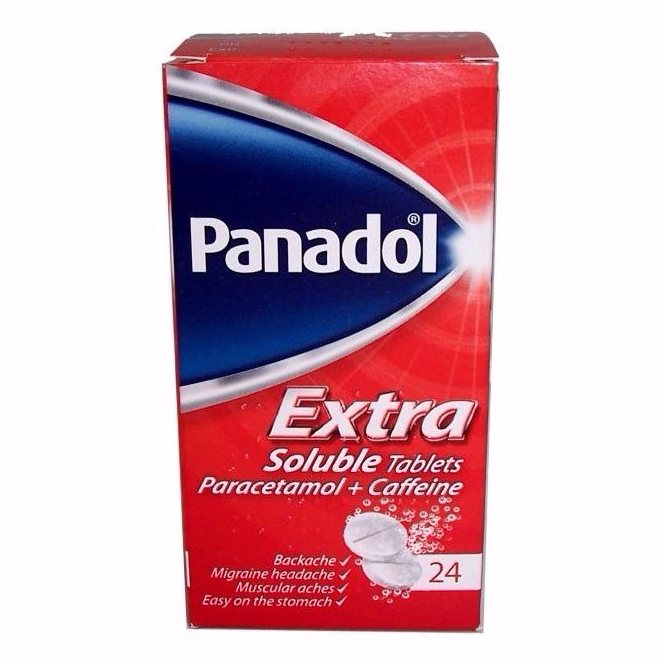
Panadol Extra contains an additional component - caffeine
Panadol Extra is especially effective for headaches caused by low blood pressure.
Quite often, pregnant women believe that achieving the maximum level of safety of treatment with Panadol is facilitated by taking a version of this drug specifically intended for children - Children's Panadol . However, the difference between this specialized product and regular Panadol is only in the reduced concentration of the active substance. Accordingly, treatment of an adult with Children's Panadol will only reduce the effectiveness of the drug.

Children's Panadol is measured using a special measuring syringe
It’s another matter if the doctor prescribed you Children’s Panadol because it is necessary to very accurately measure the dosage individually selected according to your weight, because the liquid form of the medicine allows such a calculation. This is relevant if there is a high probability of developing negative consequences from treatment.
In addition to the described forms and regular Panadol tablets, there are other varieties on sale:
- Panadol Actifast with an additional active ingredient - sodium bicarbonate (can be used during pregnancy);
- Panadol Soluble - pleasant-tasting tablets and soluble effervescent tablets (used with caution during pregnancy);
- Panadol Night Payne - with an antihistamine component (can be used during pregnancy);
- Panadol Ultra - with codeine (contraindicated during pregnancy).
There are many varieties of this medicine; different forms are sold in different countries. This is due to the need to maintain its popularity in the medicine market. Do not try to choose a drug on your own; trust your doctor to assess the risk-benefit ratio .
It's possible, just be careful
In Soviet times, when asked whether a nursing mother could take medication, the answer was categorical: either you are breastfeeding or you are sick. But at the end of the last century, WHO revised its position and, after a series of studies, decided that it is possible for a mother to take medications during breastfeeding. But be careful...
Yes, most medications pass into breast milk, but in small quantities - we are talking about only tenths. The drug reaches its peak concentration in breast milk 2–3 hours after administration. And then it is gradually eliminated from the body. So sometimes it’s enough just to separate the time between taking the pill and the next feeding - and everything will be fine.
Moreover, even the notorious ARVI is not an obstacle to breastfeeding. After all, along with mother’s milk, the baby receives not only viruses, but also antibodies to them. That is, a kind of vaccination occurs.
What to be afraid of
Forget about analgesics
. Penetrating into breast milk, they depress the baby’s central nervous system and cause hematopoiesis and kidney dysfunction.
You should not abuse acetylsalicylic acid.
If necessary, the drug can be taken once. Large doses cause an increased concentration of acid in mother's milk and can lead to metabolic disorders in the baby.
Anti-poisoning agents
should be taken with great caution. The most harmless drug for indigestion is activated charcoal. But laxatives taken by the mother will not harm the baby.
Antihistamines
also do not interfere with breastfeeding. But if necessary, choose means of only one action.
If you have an acute bacterial infection, then, contrary to popular belief, you can take antibiotics
and continue breastfeeding. The exception is sulfonamide drugs. And do not self-medicate; only a doctor can prescribe antibiotics!
Any antidepressants
should be taken only after consulting with a competent specialist. Almost all drugs in this group pass into breast milk and remain in high concentrations there for a long time. Many popular pharmaceutical herbal preparations contain alcohol, so they are not an option for you either. For irritability and nervousness, it is better to drink soothing herbal teas.
Reception tactics
The very first and most important rule is to consult a doctor about any medicine. A competent specialist must demonstrate to you not just knowledge of the instructions for use, but also the nuances: how much the drug penetrates into milk, how long it remains there, what harm is possible for the child.
Before starting medication treatment, consult your doctor: maybe they can be replaced by folk remedies? After all, instead of buying an antitussive, you can drink milk with honey. Raspberries or cranberries will help bring down the temperature. However, you should be careful with medicinal plants. For example, mint and sage help reduce lactation.
If medication is necessary, take it immediately after feeding so that the maximum concentration of the drug occurs during the break.
Paradoxically, the more often you need to take the medicine, the better it is for the baby. Give preference to those drugs that are taken not 1-2, but 3-4 times a day. The latter have a short-term effect and are eliminated more quickly from mother's milk.
Reviews from women
Paracetamol is the drug of choice during pregnancy and lactation, and, of course, as prescribed by a doctor. And Panadol is a more purified type of paracetamol, therefore less toxic. Its effect on the liver and kidneys is therefore minimal. This is written in the instructions, and the doctor explained this to me when prescribing it during pregnancy.
Anna
https://www.tiensmed.ru/news/post_new5735.html
During pregnancy I suffered from headaches. The doctor advised Panadol, only regular (not Extra). The medicine helped in 10 minutes. The pain was severe, and after 10 minutes I felt relief.
olyagol
https://otzovik.com/review_1149484.html https://lechenie-simptomy.ru/panadol-snimet-temperaturu-i-golovnuyu-bol#hcq=htHVyOp
If the cause of the headache is low blood pressure, then instead of Citramon, which is contraindicated during pregnancy due to the presence of aspirin, you can drink Panadol Extra, which contains only paracetamol, which is suitable for pregnant women, and the same caffeine as in Citramon , which makes Panadol Extra safer during pregnancy, and it helps a lot. Half a tablet is enough for me.
Alina
https://www.babyblog.ru/community/post/living/1722437#hcq=ffkWyOp
I drank Citramon during my first pregnancy (2 times), then I didn’t have an Internet connection, in fact, I didn’t even know that I shouldn’t take it. During this pregnancy, when I had a headache, I took Panadol in effervescent tablets, it relieves it immediately and is not as harmful as Citramon (it is also recommended on the Internet).
Slide
https://eva.ru/eva-life/messages-2641488.htm
I took Panadol during pregnancy, it was the only thing that helped me, no more than 2 tablets a day. Headaches cannot be tolerated at all.
TO
https://www.askmamas.ru/answers.php?qid=33229
Paracetamol is a dummy, it doesn’t take me at all, I don’t know, I was in storage 1.5 weeks ago, the doctor said about Citramon that it could cause bleeding! And Panadol Extra contains paracetamol and a little caffeine, just for those suffering from low blood pressure).
L
https://www.askmamas.ru/answers.php?qid=33229
Example and life
Natalia, 35 years old, Krasnogorsk:
My daughter was six months old when my hands became covered with eczema. I was prescribed hormonal ointments and injections. And the dermatologist strictly told me to stop breastfeeding.
When my son was born 5 years later, history repeated itself. But either during this time something changed in our medicine, or I just happened to have a conscientious doctor, but I was prescribed modern hormonal creams and... allowed to continue breastfeeding the baby. Then I repeated the course of treatment with these creams a couple of times. And she successfully fed the boy for more than a year.