Breast milk is the first food of a newborn baby, containing everything necessary for him. Breastfeeding is the key to the health and proper development of a child from the very first days of life. Contrary to popular belief, breast milk is not a sterile body fluid and contains bacteria, both opportunistic and beneficial, the balance between which is sometimes disturbed and then there is a need to analyze breast milk for microflora.
A correct understanding of the sterility of breast milk does not imply the absolute microbiological purity of breast milk, but the absence in it of harmful, pathogenic bacteria that can harm the baby by disrupting the functioning of the gastrointestinal tract, or undermine the health of the mother.
Composition of microflora - norm and pathology
The normal microbiota of breast milk includes: staphylococci, streptococci, lactic acid bacteria, propionic bacteria, bifidobacteria, etc. The predominant opportunistic microorganisms in breast milk are bacteria of the genus Staphylococcus (S. epidermidis), golden (S. aureus) and saprophytic (S.saprophyticus), other microflora are found in smaller quantities: the genus Streptococcus, the genus Enterococcus, etc. Such bacteria can provoke the inflammatory process only with certain changes developing in the body. The greatest danger is posed by Staphylococcus aureus, which, thanks to its protective shell, can penetrate cells without damage and destroy them with its poisons.
Where do the bacteria in breast milk come from?
Thanks to recent research, it has been found that human milk is a source of bacteria for colonizing the baby's intestines. The necessary microflora begins to form in the mammary glands during pregnancy and then during lactation. The composition of microorganisms in each woman's milk is different and subject to change.
The source of lactic acid bacteria, propionic bacteria and bifidobacteria in the mammary glands, according to some assumptions, is the mother's intestines. Staphylococci and other opportunistic bacteria always live on the mucous membranes and skin of humans. Their penetration into milk from the skin of the nipples occurs at the moment the baby expresses or sucks the breast.
The reason for excessive growth of opportunistic microflora can be a number of reasons:
- significant weakening of the immune system of a nursing woman;
- exacerbation of an existing chronic disease;
- nervous or physical exhaustion;
- period after surgery.
Bacteria can enter breast milk in the following ways:
- through microtraumas and cracks in the nipples;
- internally during a sore throat or flu;
- in case of non-compliance with personal hygiene rules.

What microorganisms are in milk?

• skin pustular infections; • intestinal dysbiosis; • frequent colds; • developmental delay; • disruption of the digestive system.
If mother's milk is significantly contaminated with opportunistic or pathogenic microorganisms, then mastitis will be a complication of lactation. In this case, purulent discharge appears from the nipple, the breast swells and hurts greatly. The inflammatory process occurs against the background of an increase in temperature to 38-39 C, with chills.
There is evidence in the literature that breast milk contains more than 700 species of bacteria, most of which are lactic acid. Moreover, some types of bacteria are unknown to scientists. After six months, the composition of the milk changes, which makes it possible for other microorganisms to colonize the baby’s intestines.
Whether it is possible to breastfeed if there are bacteria in the milk depends on their number and properties. If the mother does not have any inflammatory processes, but microorganisms are found in the milk, breastfeeding can and should be done.
We suggest you read: Baby's eye twitches
If a child has mastitis, it is recommended to apply it to a healthy mammary gland.
If, according to the results of the study, staphylococcus has been cultured and there are clinical manifestations of infection, antibacterial therapy is indicated, taking into account sensitivity to the pathogen.
• protected penicillins; • cephalosporins; • macrolides.
To restore beneficial microflora in the body, eubiotics are used, which populate the intestines with beneficial bacteria and create favorable conditions for the growth and reproduction of “good” microorganisms. Such biologically active supplements can be given to children from the first days of life if there is a need for antibiotics for the nursing mother or the child himself.
• Conjunctivitis (inflammation of the conjunctiva of the eyes: redness of the eyelids, the appearance of purulent discharge, swelling, pain). • Omphalitis (inflammation of the navel). • Enterocolitis (inflammatory process in the gastrointestinal tract: abdominal pain, diarrhea, stool with blood and mucus, vomiting and nausea); • Staphyloderma (appearance on the skin of specific blisters filled with pus, skin itching, hyperemia). • Sepsis. • Cellulitis and abscesses.
In order for a child to develop the diseases described above, the action of the microbe alone is not enough; a malfunction of the immune system and an additional source of infection are necessary.
Important! A test for staphylococcus should be performed if the child has pyoderma (pustular skin lesions).
As with any purulent-inflammatory processes, the general condition suffers, which is manifested by increased temperature, refusal to eat, anxiety, crying, lethargy, and sleep disturbances. After antibiotic therapy, the condition normalizes.
When is verification necessary?
An analysis of breast milk for sterility must be done when a woman is going to become a breast milk donor, if the woman is diagnosed with purulent mastitis, or if the baby itself has symptoms indicating an infection.
A bacterial infection in a baby can be recognized by the following signs:
- rashes on the surface of the skin with purulent formations;
- loose stools with mucus and greens;
- flatulence;
- intestinal disorder;
- increase in body temperature.
With purulent mastitis, the mother is concerned about the following symptoms:
- the mammary glands become hard;
- the tissue in the chest area turns red and swells;
- purulent discharge appears from the nipples;
- body temperature rises.
Important! Purulent mastitis is a contraindication to breastfeeding.
Analysis of milk sterility allows not only to identify pathogenic microorganisms that led to the inflammatory process, but also to determine their sensitivity to antibiotics.
What is a breast milk test called?
Before donating breast milk for analysis, the mother must clearly determine the need for this procedure. There are several ways to carry out such diagnostics, depending on the goals. This biological product is often tested for:
- sterility;
- fat content;
- presence of antibodies.
We suggest you read Allergy to cow protein in infants: symptoms and how milk intolerance manifests itself in a child
This technique is necessary to exclude the presence of harmful microorganisms. They can penetrate either from the outside or move from the source of inflammation in the woman’s body along with the blood flow. This analysis of breast milk identifies the specific type of microorganism and determines its concentration. Based on the results obtained, medications are prescribed. The interpretation of the microflora analysis of breast milk is carried out exclusively by a doctor. The presence is often recorded:
- staphylococcus;
- enterobacteria;
- candida mushroom;
- Klebsiella
The study is mandatory in the presence of inflammatory and infectious processes in the gland. Accurate identification of the causative agent helps to quickly begin effective therapy and eliminate symptoms and manifestations of the disease. The nursing woman herself should be interested in its purpose. The difficulty of implementation is often due to the lack of necessary equipment and personnel.
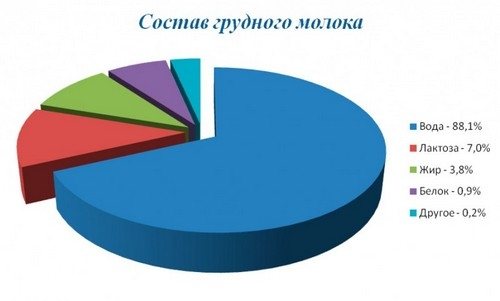
This type of test determines the presence of fats. Such elements are difficult to digest. Because of this, babies often have digestive problems. Analysis of breast milk for composition also involves determining the degree of fat content. In this case, for testing it is necessary to collect only the biological material that is released approximately 2-4 minutes from the start of pumping. For collection, you must use clean, washed and sterilized containers.
The resulting material is poured into a test tube. It has a notch, which is located 10 cm from the bottom. After waiting 6 hours, the result is assessed. After this time, a layer of cream forms on the surface. It is important not to shake the container during the test. When assessing the results after analyzing breast milk, it is considered that 1 mm of creamy layer corresponds to 1% fat content.
This method is often used to determine the causes of mastitis during lactation. It can develop as a result of stagnation or penetration of pathogenic microorganisms through cracks in the nipple. In order to have breast milk tested for staphylococcus, a woman collects it into a sterile container. The resulting sample is sent to the laboratory.
It is carried out in the presence of Rh conflict - a disorder in which the Rh factor of the mother and child do not match. To exclude the possibility of antibodies passing from the mother’s body to the baby, doctors advise stopping breastfeeding or waiting until the baby is one month old. This fact can be excluded by conducting a test.
Symptoms of infection in a child
Staphylococcus aureus is most often found in breast milk. When it penetrates the mammary gland, it can cause purulent mastitis in a nursing mother, and cause diseases such as in a child:
- enterocolitis (frequent loose stools with mucus or greens, increased body temperature, vomiting);
- rashes on the surface of the skin with purulent formations;
- intestinal dysbiosis (flatulence, regurgitation, changes in the color and consistency of stool).
Important! Staphylococcus aureus is highly resistant to many antibacterial drugs, so it is not always possible to deal with it quickly.
Similar intestinal disorders can be caused by E. coli, Klebsiella, and Candida fungi.
Where can I submit it?
A woman can do an analysis for the sterility of breast milk herself by choosing one of the laboratories that provide such a service, or by first contacting her local doctor, who will issue a referral. The following laboratories perform this analysis.
- Laboratory Invitro. The cost of the analysis is 815 rubles. It can be done either in the laboratory or with its employees visiting your home. The duration of the study takes no more than four days.
- International medical center On Clinic. The cost of such a service is 750 rubles, the result is ready on the fifth day.
- Clinic of Modern Medicine IAKI. Sowing for flora will cost 1,800 rubles. The duration of the study takes three days.
- Medical laboratory Hemotest. The execution time is 5 days, the cost of analysis is 1200 rubles.
How to pass it correctly
To get the most accurate result of a breast milk sterility test, you must try to ensure that no bacteria from the skin gets into the sample. To do this, you will need special sterile containers, such as test tubes. You can buy dishes at the pharmacy or sterilize two small jars. You need two of them - one for each breast.
Before you start collecting milk, you need to thoroughly wash your hands and breasts with soap, and the areola area can even be wiped with an alcohol solution or a special sterile cloth. After this, start expressing milk. The first portion should be decanted into the sink, and the second into a container prepared for this purpose. The milk sample must be delivered to the laboratory as soon as possible, at the latest within 2-3 hours after collection. If you take the test later, the result may be incorrect.
The study itself usually lasts at least a week. The reason for this is that it is during this period that bacterial colonies have time to grow and multiply. After this, the specialist studies the qualitative and quantitative composition of microorganisms, and can also draw conclusions regarding the resistance of microorganisms to antibiotics and antiseptics. This will allow you to choose the most effective medications if the doctor decides that this microflora needs to be gotten rid of.
How to assemble correctly
To ensure that the analysis of breast milk for sterility is as accurate as possible, it is important to correctly collect the material for subsequent research. To do this, you must follow the following instructions.
- First, you should purchase a special container from the pharmacy, where breast milk will then be placed.
- Milk from the right and left glands cannot be mixed together.
- Two weeks before milk collection, you should stop taking medications.
- Before the pumping procedure itself, you should thoroughly wash your hands with soap and treat the nipple area with medical alcohol. Do not forget that each nipple is treated with a separate cotton pad.
- When you start expressing milk, you just need to pour the first 10 ml into another container. Such material is not suitable for analysis.
- The remaining volume of milk is expressed into a purchased container, which is tightly closed with a lid. It is important not to touch the edges of the container with your body during the procedure.
- When closing containers, you must also ensure that your hands do not touch their walls. Then the containers are signed. They indicate the woman’s personal data, and also make a note from which breast the milk was taken.
The collected material must be delivered to the laboratory no later than four hours. All this time it should be stored in the refrigerator. You cannot donate milk that was collected the day before, or if it was placed in an unsterile container.

How to properly collect milk for analysis?
To collect milk for analysis, follow these recommendations:
- Prepare two glass or plastic disposable jars for analyzing breast milk - there should be separate containers for the left and right breasts.
- Boil glass jars with lids for 10 - 12 minutes; just wash plastic ones with warm water.
- Make a mark on each container for the left and right breast.
- Wash your hands and breasts with warm water and baby soap.
- The first milk supply is not suitable for culture, so first express 10 ml from each breast into the sink and rinse the breasts again.
- Dry your breasts with a clean cloth.
- After this, express 10–15 ml from each gland into prepared jars and close them with lids.
- Very quickly deliver or take the jars of milk to the laboratory. Breast milk analysis should be done no later than 3 hours from the moment of expression.
A woman needs to be extremely careful when collecting milk for sowing. Bacteria from skin or clothing should not enter it.
In the laboratory, milk samples are sown on nutrient soil, where microorganisms grow rapidly. Simultaneously with determining the type and number of bacteria, their resistance to antibiotics is determined.
Expressing milk for testing
Decoding, norms, what shows
When examining breast milk in laboratory conditions, the following can most often be detected:
- Staphylococcus (Staphylococcus). Epidermal staphylococci with strong immunity cannot cause harm. But when it weakens, they provoke rashes on the baby’s skin surface. Staphylococcus aureus can cause pneumonia, meningitis and osteomyelitis. Saprophytic staphylococcus rarely affects children.
- Klebsiella. A representative of the genus Enterobacteriaceae, which affects certain organs and tissues. Most often this concerns the lungs, intestinal tract, and genitourinary system. When they get into milk, the child begins to have problems with the respiratory tract and nasopharynx, and can also develop gastritis and enterocolitis.
- Streptococcus (Streptococcus). May provoke the development of intestinal infection.
- Pseudomonas aeruginosa (Pseudomonas aeruginosa). A rod-shaped bacterium that becomes dangerous when the immune system is weakened. It affects the urinary tract system as well as the intestinal tract, causing abscesses.
- Escherichia coli. A representative of the genus Enterobacteriaceae, which provokes acute intestinal poisoning, can cause sepsis, mastitis and meningitis.
- Serratia. A genus of conditionally pathogenic enterobacteria, most often capable of affecting the respiratory system, gastrointestinal tract and genitourinary system. In small quantities it is not dangerous, in large quantities it can cause the milk to turn pink.
- Non-fermenting bacteria (Pseudomonas, Acinetobacter). Bacteria that are not capable of carrying out fermentation processes. Most often they are caused by nosocomial infections.
The very fact of detection of opportunistic microflora is not yet a reason to prescribe antibiotic treatment and stop breastfeeding. What is more important here is how many microorganisms were detected and whether their growth was observed. The results of the analysis may vary depending on this.
- No growth of opportunistic organisms was detected. In this case, we can talk about the sterility of breast milk and its safety for the baby and mother.
- Slight growth of Staphylococcus epidermidis or Enterococcus was detected. Non-mass growth of bacteria is considered to be less than 250 CFU/ml. This is also a completely normal result and the mother can continue breastfeeding.
- The growth of Staphylococcus aureus, Pseudomonas aeruginosa, and Escherichia coli was detected. Mass bacterial growth is defined as growth of more than 250 CFU/ml. Such a result with obvious signs of mastitis in a woman requires immediate treatment with antibacterial drugs.
Treatment of infection in mother and child
As soon as the breast milk tests are ready, they need to be shown to your doctor. He will be able to decipher the tests, make a diagnosis and, if necessary, prescribe appropriate treatment.
If a bacterial infection is detected in milk, the woman is prescribed antibacterial therapy. At this time, breastfeeding is stopped, and the milk is expressed to preserve lactation in the future. It is recommended to treat nipples with antiseptic solutions. Medicines that normalize intestinal microflora may also be prescribed. Vitamin complexes are prescribed to enhance immunity.

If the child also shows signs of infection, then he, like the mother, is prescribed antibacterial therapy.
Important! Dr. Komarovsky, if a mother detects Staphylococcus aureus in breast milk without signs of mastitis, advises not to stop breastfeeding and start taking antiseptic medications. The child is prescribed probiotics.
If a small amount of enterococcus or staphylococcus epidermidis is detected in breast milk, then do not panic. In small quantities, these bacteria are not harmful and do not threaten the baby’s health. The baby can continue to be attached to the breast. It is important to maintain personal hygiene during this period, especially during breastfeeding.
Mother's milk is complete nutrition for the baby, on which its normal development depends, but if a woman notices unpleasant symptoms, or the baby has persistent intestinal disorders, breast milk should be tested for sterility.
Treatment of staphylococcal infection and its consequences
If mastitis in a nursing woman does not become purulent, then treatment can be carried out with folk remedies. For example, apply a scalded cabbage leaf to your chest or make a compress with a saline solution - dissolve 1 tablespoon of salt in a glass of warm water. If a woman is unable to cope with mastitis, it can turn purulent.
If purulent mastitis is detected in a nursing woman, it is imperative to consult a doctor and undergo appropriate treatment, including antibiotics. The doctor will select a drug that will be as safe as possible for the child. If a nursing woman does not take antibiotics, this can lead to fistulas, breast deformation, and sepsis. When it is impossible to select an antibiotic that would not have a significant effect on the child’s health, breastfeeding is stopped.
- How to pump breasts when milk is stagnant
- Testing breast milk for sterility